Caren G. Solomon, M.D., M.P.H., Editor
Tamara S. Hannon, M.D., and Silva A. Arslanian, M.D.
This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal guidelines, when they exist. The article ends with the authors’ clinical recommendations.
A 12-year-old boy with excessive weight gain that began when he was approximately 6 years of age presents for evaluation of obesity. He occasionally rides his bicycle but spends more than 6 hours per day engaging in screen-based activities (e.g., video games and social media). He drinks sugary beverages every day and eats mostly processed foods. His mother has obesity, and his maternal grandmother has type 2 diabetes. His body mass index (BMI, the weight in kilograms divided by the square of the height in meters) is 41.9 (class 3 obesity, ≥140% of the 95th percentile for his age and sex). The fasting cholesterol level is 202 mg per deciliter (5.23 mmol per liter), low-density lipoprotein (LDL) cholesterol level 127 mg per deciliter (3.29 mmol per liter), triglyceride level 320 mg per deciliter (3.62 mmol per liter), and high-density lipoprotein (HDL) cholesterol level 43 mg per deciliter (1.11 mmol per liter). The glycated hemoglobin is 5.9% (6.8 mmol per liter), which is consistent with prediabetes. The alanine aminotransferase level is 80 U per liter, with hepatic steatosis shown on ultrasonography. How would you manage this case?
KEY CLINICAL POINTS
Obesity in Adolescents
- Adolescent patients with obesity benefit from evaluation and follow-up according to a long-term care model with attention to and understanding of the societal stigma and pervasive weight bias that exists around obesity.
- Obesity during adolescence is associated with a substantial increase in the risk of concurrent and later health consequences that should be evaluated and treated expediently.
- Intensive treatment with regard to health behavior and lifestyle, with at least 26 hours of face-to-face treatment over a period of at least 3 months, is a foundational aspect of the comprehensive treatment of obesity.
- The elimination of sugar-sweetened beverages from the patient’s diet is strongly recommended.
- The use of antiobesity medications or bariatric surgery (or both) along with intensive treatment with regard to health behavior and lifestyle results in a greater reduction in body-mass index than lifestyle treatment alone and should be discussed with families, along with the caveats that weight regain is common, data regarding long-term outcomes are lacking, and these treatments are expensive.
The Clinical Problem
Obesity during adolescence (10 to 19 years of age) is associated with health consequences that include prediabetes and type 2 diabetes,1 nonalcoholic fatty liver disease,2 dyslipidemia,3 polycystic ovary syndrome (PCOS),4 obstructive sleep apnea,5 and mental health disorders and social stigma.6 In addition, obesity during adolescence is a risk factor for complications and death from coronary heart disease7,8 as well as for death from any cause in adulthood,8 including early adulthood.9
In a study involving 2.3 million persons in Israel, BMIs in late adolescence that were between the 85th and 94th percentiles and above the 95th percentile were associated with hazard ratios for sudden death and for death from coronary heart disease or stroke during adulthood of 2.2 and 3.5, respectively.8 Although these associations were not adjusted for BMI in adulthood, other data indicate that decreasing adiposity between childhood and adulthood is associated with reductions in cardiometabolic risk factors.10 In addition, combined data from four prospective cohort studies showed that elevated BMIs in both childhood and adulthood were associated with increased relative risks for type 2 diabetes (relative risk, 5.4), hypertension (relative risk, 2.7), elevated LDL cholesterol levels (relative risk, 1.8), and carotid artery atherosclerosis (relative risk, 1.7), whereas persons with elevated childhood BMI and normal adult BMI had risks for these conditions that were similar to those among persons with normal childhood and adult BMIs.10 These studies support the importance of diagnosis and treatment of obesity during childhood and adolescence, as well as in adulthood, to reduce adverse health consequences.
The prevalence of obesity in adolescents has increased since the 1980s, most markedly in low-income communities and communities of color, a difference that is at least in part attributable to structural racism and stigma (with negative attitudes creating social and economic obstacles to health).11 Among the social drivers of obesity is the marketing of unhealthy foods and drinks.12 In the United States, the prevalence of obesity in the 2015–2016 period was 20.6% among adolescents (as compared with 14.8% in the 1999– 2000 period) — 22.0% among non-Hispanic Black adolescents and 25.8% among Hispanic adolescents, prevalences that are higher than those among both non-Hispanic White adolescents (14.1%) and non-Hispanic Asian adolescents (11.0%).13
Rates of weight gain accelerated during the coronavirus 2019 (Covid-19) pandemic; a retrospective cohort study in California showed an absolute increase in the prevalence of overweight or obesity of 5.2 percentage points among 12-to-15-year-olds and 3.1 percentage points among 16-to-17-year-olds during the first year of the pandemic.14 Moreover, obesity is among the most common underlying conditions for COVID–19–associated death in persons younger than 21 years of age.15 Obesity interventions are needed to improve health in adolescence and beyond.
Strategies and Evidence
ASSESSMENT
BMI is strongly associated with adiposity and is a useful clinical tool for assessing overweight and obesity, although its use has limitations.16 Higher BMI in some cases reflects increased lean body mass, and in Asian populations, adiposity is increased at lower BMI levels.17 In adolescents, a BMI at or above the 85th percentile but below the 95th percentile is diagnostic of overweight, and a BMI at or above the 95th percentile is diagnostic of obesity.18 Class 1 obesity is defined as a BMI at or above the 95th percentile up to 119% of the 95th percentile, class 2 obesity is a BMI at or above 120% of the 95th percentile up to 139% of the 95th percentile, and class 3 is a BMI at or above 140% of the 95th percentile. 18 As an adolescent’s final height is reached, adult thresholds for overweight (BMI, 25) and obesity (BMI, 30) apply. Severe obesity in children is defined as class 2 or 3 obesity or a BMI of 35 or higher.16,18
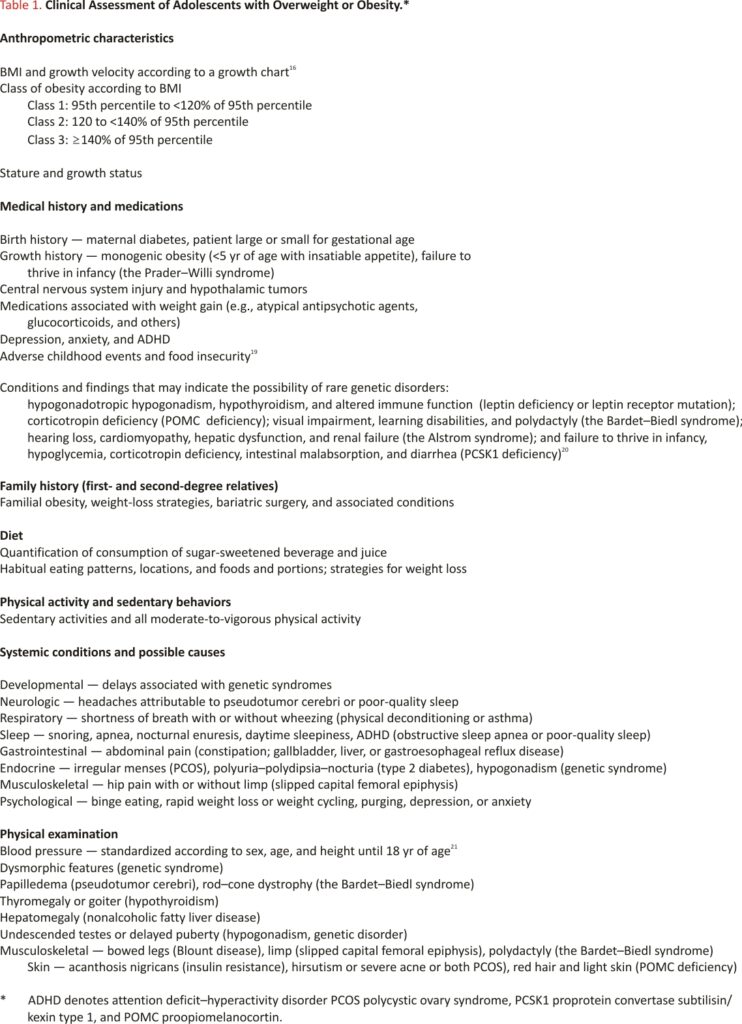
An evaluation of obesity in an adolescent includes complete medical and medication histories and a family history. The evaluation should include an assessment of obesity-related diseases and lifestyle factors as well as environmental and social factors, a psychosocial assessment that includes screening for depression (with the use of the Patient Health Questionnaire-9 for Teens), and a physical examination (Table 1).3,18-21 Eliciting a family history of obesity-related conditions, including premature deaths due to cardiovascular disease or stroke, is important for assessment and discussion of familial risk.3
LABORATORY ASSESSMENT
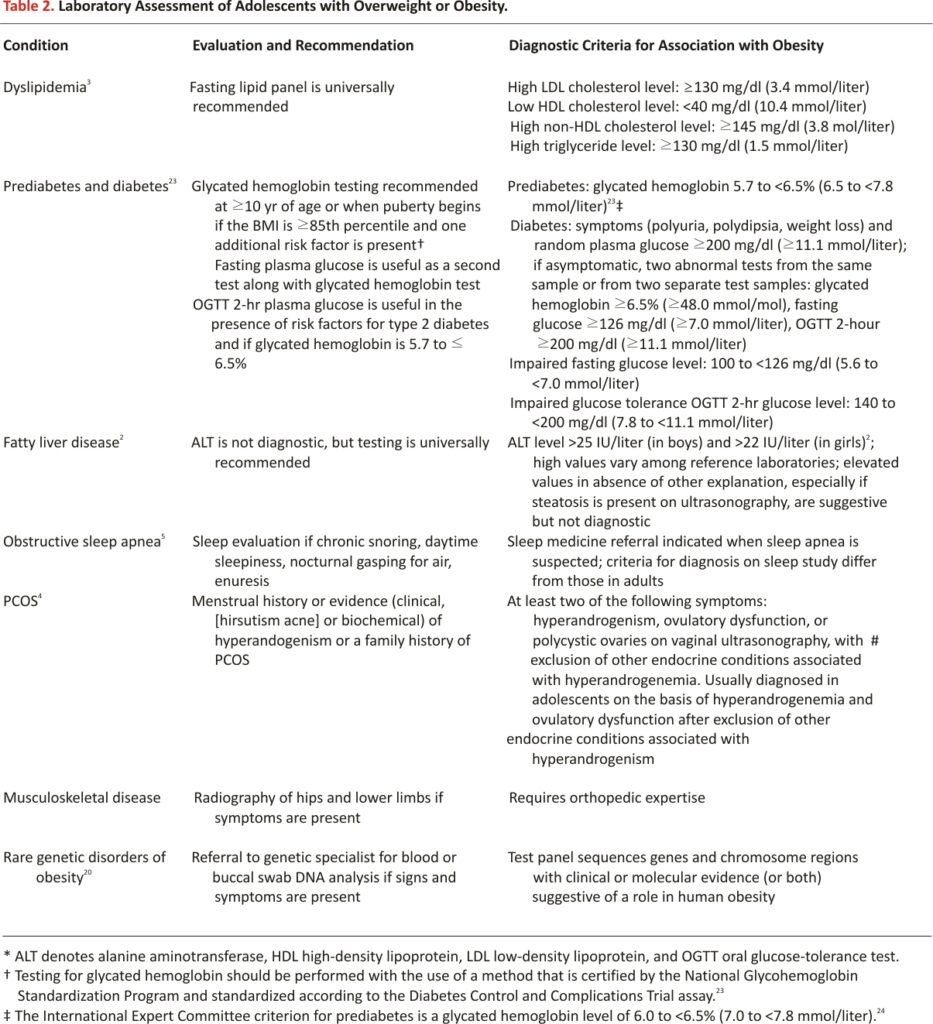
Table 2 shows recommendations for laboratory tests in adolescents with obesity, including screening for dyslipidemia3 and fatty liver disease.2 Consistent with guidelines of the Pediatric Endocrine Society and the American Diabetes Association, screening for type 2 diabetes is recommended in adolescents who have a BMI at or above the 85th percentile and one additional risk factor: family history of type 2 diabetes in a first- or second-degree relative, non-White race or ethnic group, physical signs or conditions associated with insulin resistance (e.g., acanthosis nigricans, hypertension, dyslipidemia characterized by low levels of HDL cholesterol and high levels of triglycerides, and PCOS), gestation complicated by diabetes, or intrauterine growth restriction.22,23 The possibility of autoimmune type 1 diabetes against the backdrop of obesity should be considered, and measurement of diabetes-associated antibodies against glutamic acid decarboxylase, insulinoma-associated protein 2, and zinc transporter 8 is recommended.23 Criteria for the diagnosis of diabetes and prediabetes are shown in Table 2. Glycated hemoglobin testing is a poor predictor of elevated fasting glucose levels and 2-hour results of an oral glucose tolerance test and may be insufficient to diagnose early type 2 diabetes or accurately reflect prediabetes.25 In patients with multiple risk factors for type 2 diabetes and a glycated hemoglobin level of 5.7% to less than 6.5% (6.5 to <7.8 mmol per liter), an oral glucose tolerance test is useful for the detection of early type 2 diabetes.22
Additional evaluations rely on clinical findings (Table 2).4,5 Persistently elevated levels of liver enzymes (for >3 months) may prompt further evaluation for nonalcoholic fatty liver disease.2 Laboratory evaluations for endocrine disorders that are associated with increased adiposity, including hypothyroidism and Cushing’s syndrome, are not recommended unless there is growth attenuation or other clinical indications. In addition, the measurement of insulin concentrations to evaluate insulin resistance adds no diagnostic value and is not recommended. The diagnosis of suspected genetic obesity syndromes requires medical genetics evaluation and often additional workup, including karyotype analysis and DNA methylation studies.20 Although only a small percentage of cases of pediatric obesity is attributable to a monogenic cause, testing for monogenic causes of obesity is indicated in cases of insatiable appetite and severe obesity in children younger than 5 years of age.
MANAGEMENT
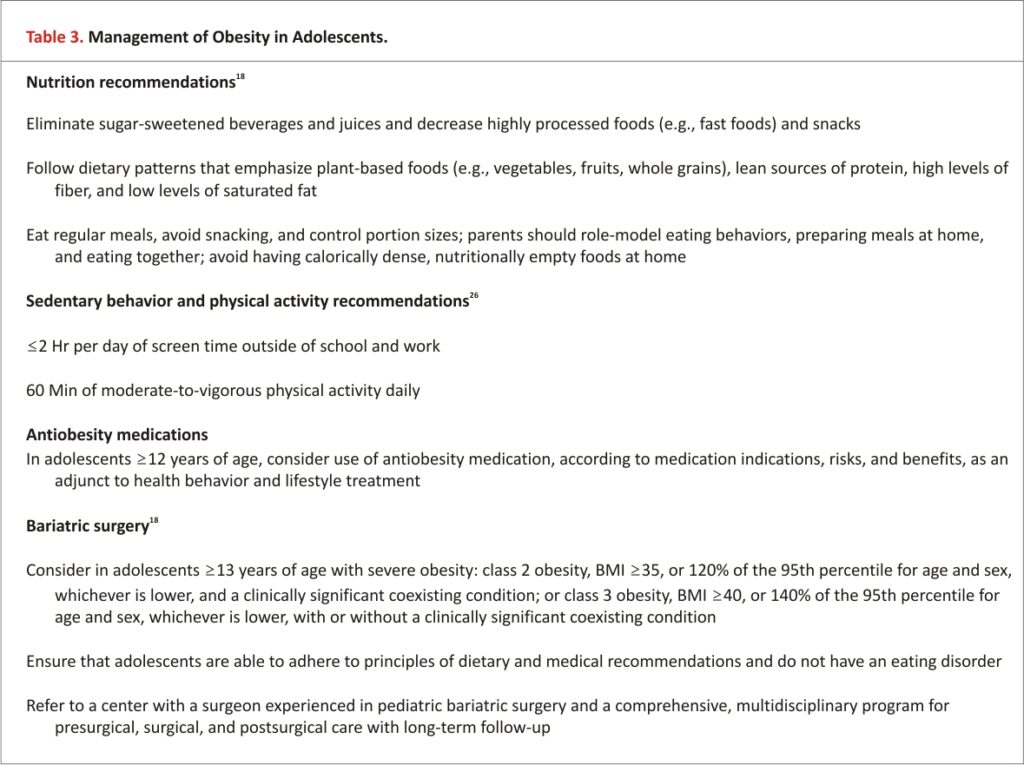
Management of obesity in adolescents should use a multidisciplinary long-term care model that includes attention to lifestyle modification and consideration of pharmacologic and bariatric surgical therapies (Table 3 and Table 4).18 Communication should be considerate of the stigma associated with the term “obesity,” and the use of person-first language (i.e., “person with obesity” rather than “obese person”) and preferred terms such as “too much weight for age (or health or height)” is important. 6,18 Motivational inter-viewing may be useful as part of a multidisciplinary approach; a meta-analysis of 11 randomized trials assessing the use of this technique in adolescents with obesity indicated some positive effects on nutrition, physical activity, and quality of life, although with no significant reductions in BMI or cardiometabolic outcomes.27 Patients with symptoms of depression or other mental health disorders should be referred to a behavioral health provider.
Lifestyle Interventions
Summary data from randomized, controlled trials of lifestyle treatment approaches indicate that interventions that offered at least 26 hours of face-to-face counseling regarding nutrition, physical activity, and lifestyle recommendations resulted in, on average, modest but clinically important changes in the mean BMI z score (at least −0.15 to −0.25; the z score represents the number of standard deviations by which the BMI differs from the mean in a reference sex- and age-matched population). Evidence was not adequate to support the recommendation of treatment with less intensive interventions (Table 3).28
Dietary Interventions
Sugar-sweetened beverages, the leading source of added sugars in the diets of children and adolescents in the United States, contribute to obesity and additional health risks in adolescents and should be eliminated from the diet, given that such beverages lack any nutritional value.29 A meta-analysis of prospective observational studies indicated that over the course of 1 year, each additional 12-oz (0.35-liter) daily serving of sugar-sweetened beverage was associated with a BMI increase of 0.06 (95% confidence interval, 0.02 to 0.10, as calculated with the use of a random-effects model).30
Dietary patterns that emphasize plant-based foods (i.e., vegetables, fruits, and whole grains), lean sources of protein, high fiber intake, and low consumption of saturated fat are associated with better cardio-metabolic risk profiles. Ketogenic diets, which are used for treating some seizure disorders in children, have been incorporated into some obesity treatment programs for adolescents and have shown short-term safety and efficacy (weight loss of 7 to 9% of the baseline body weight at 3 to 4 months of follow-up).31 However, these programs have substantial attrition, and there is insufficient data to inform long-term outcomes with these diets or with low-carbohydrate diets in adolescents.
Supervised marked caloric restriction (very low-calorie diets) for weight loss in adolescents is not recommended. Studies have shown mixed results with the use of these diets; weight regain is typical,32 and there are concerns regarding long-term acceptability and safety, including risks of eating disorders, electrolyte or other metabolic disturbances, vitamin and mineral deficiencies, and adverse psychological effects.33 Although the social emphasis on patient-imposed restrictive dieting behaviors is associated with a risk of disordered eating, supervised multidisciplinary weight management and treatment of obesity with ongoing support from a pediatrician, pediatric dietician, and mental health professional are not associated with an increased risk of eating disorders.34
Physical Activity Interventions
Dose–response studies of physical activity in adolescents indicate that benefits with regard to adiposity and cardiorespiratory and cardiometabolic measurements are observed with a daily average of 60 minutes of physical activity at a moderate-to-vigorous level of intensity.26 Randomized trials of supervised interventions of shorter durations of moderate-to-vigorous aerobic exercise or combined aerobic and strength training (median, 3 days per week for 40 minutes per session) have also been shown to result in clinically significant cardiometabolic benefit and reductions in percent body fat (by approximately 5 to 6%).35,36
Multidisciplinary Interventions
A review of 28 randomized, controlled trials of multidisciplinary interventions of varying content (combinations of diet, physical activity, and behavior modification) and duration without pharmacotherapy in 2774 adolescents with obesity indicated only limited efficacy, with a mean difference in BMI of 1.18 with intervention as compared with control after at least 6 months of follow-up.37 Although participants reported high levels of satisfaction with the interventions and improved quality of life, the potential effect of reporting bias, attrition, and variable adherence on overall outcomes of multidisciplinary interventions is difficult to assess.
Antiobesity Medications
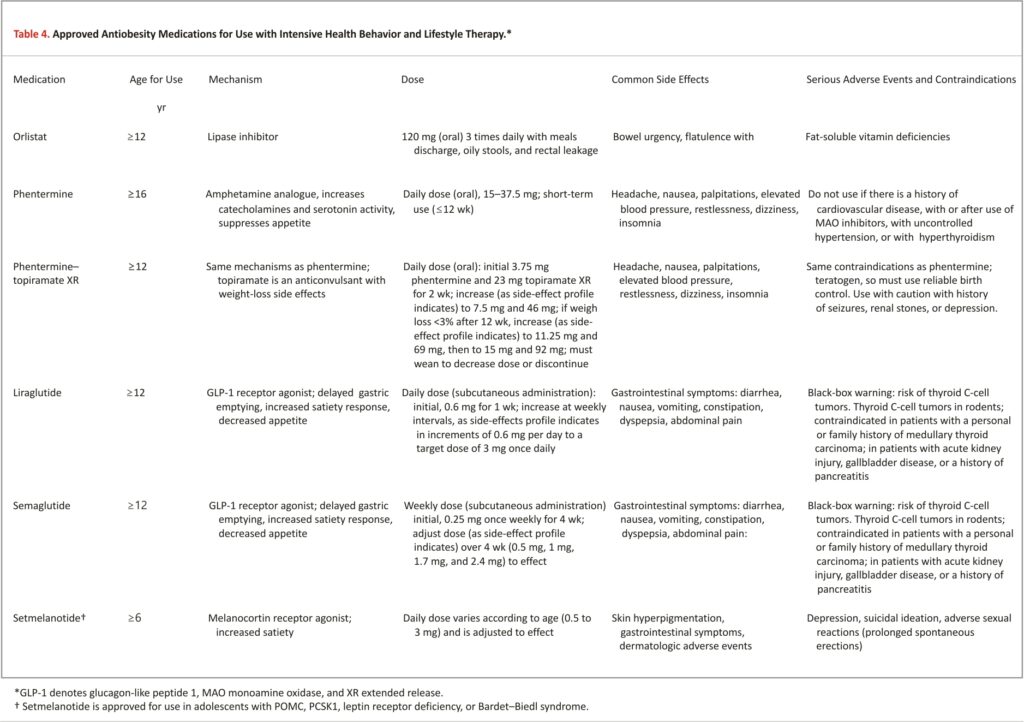
The addition of approved weight-loss medications has improved the outcomes of multidisciplinary weight-loss programs in clinical trials.38-40 Antiobesity medications that have been approved by the Food and Drug Administration for use in adolescents are shown in Table 4. Orlistat, a lipase inhibitor, is associated with flatus, oily spotting, fecal urgency, and incontinence — side effects that limit use in adolescents.41 Phentermine, an amphetamine analogue that suppresses appetite, is approved for short-term use (≤12 weeks) in adolescents older than 16 years of age and is approved in combination with topiramate in adolescents at least 12 years of age when accompanied by counseling that topiramate is a teratogen and information regarding appropriate contraception.40,42
Randomized, placebo-controlled trials have shown the effectiveness of two glucagon-like peptide 1 (GLP-1) receptor agonists – liraglutide and semaglutide – in adolescents when combined with lifestyle therapy. In one placebo-controlled trial, liraglutide (administered subcutaneously at a dose of 3 mg daily) resulted in a greater reduction in the BMI (estimated difference, −4.6%) and body weight (estimated difference, −4.5 kg) at 56 weeks of treatment.38 In another placebo-controlled trial, semaglutide (administered subcutaneously at a dose of 2.4 mg once weekly) resulted in a greater reduction in BMI (−16.7%) and body weight (−17.7 kg) at 68 weeks, as well as greater reductions in waist circumference and levels of glycated hemoglobin, lipids (except HDL), and alanine aminotransferase.39 Both agents are approved for indefinite use in adolescents 12 years of age and older. The major adverse effects are gastrointestinal symptoms; key contraindications include a personal or family history of medullary thyroid carcinoma, acute kidney injury, gallbladder disease, or pancreatitis.
Metformin is frequently administered off-label for obesity in adolescents. In a meta-analysis of 38 randomized trials involving children or adolescents (2199 participants; mean age, 13.7 years; daily dose range, 500 to 3000 mg; duration, 12 to 192 weeks), metformin reduced the mean BMI by 1.1 as compared with controls.43 Topiramate, an anti-convulsant that is used for migraine prophylaxis, is also prescribed off-label for obesity after observations of dose-dependent weight reduction as a side effect among patients who received it.40
There is insufficient evidence to support antiobesity medication as monotherapy in adolescents without a multidisciplinary treatment strategy. Given the chronic nature of obesity, BMI is expected to increase after discontinuation of antiobesity medications. After participants had a 6-month withdrawal from liraglutide in a randomized trial of liraglutide, the difference in the BMI from baseline was less than 2%.38 Because anti-obesity medications are associated with substantial cost, adverse effects, and a still-uncertain benefit–risk ratio over the long term, discontinuation of the medication is suggested if there is no BMI reduction after administration at therapeutic dose levels for 4 months. A trial of a different medication may be considered.
Bariatric Surgery
In a cohort study involving adolescents, bariatric surgery (Roux-en-Y gastric bypass and vertical sleeve gastrectomy) was associated with weight loss of approximately 26% of the baseline body weight at 5 years (Table 3).44 Remission rates 5 years after surgery were approximately 86% for type 2 diabetes and 68% for hypertension.44 A randomized, controlled trial of surgical treatment as compared with nonsurgical treatment (8 weeks of low-calorie diet) in Sweden showed a 2-year change in BMI of −12.6 and −0.2, respectively.45
Most postsurgical complications are mild, but up to 8% of adolescents have major perioperative complications.44 Long-term complications include deficiencies in nutrients (e.g., iron, vitamin B12, and folate), reduced bone mass, and weight regain.44 The incidence of alcohol-use disorders has also been reported to be higher among adolescents after metabolic and bariatric surgery, 46 although whether the disorders occur more commonly in adolescents with obesity who undergo surgery than in those who do not is unclear. Weight regain after surgery varies; approximately 60% of adolescents who were followed for 5 years after undergoing gastric bypass maintained a reduction from the baseline body weight of at least 20%, whereas 8% regained at least 95% of the initial weight lost.44 Important predictors of weight regain among adolescents after surgery include younger age and lack of presurgical weight loss.47
Areas of Uncertainty
Questions remain with regard to why the prevalence of obesity continues to increase and the effects of environmental drivers (e.g., pollution and polyfluoroalkyl substances). The extent to which the increasing use of antiobesity medications (including more potent medications, such as dual-agonist peptides [tirzepatide], that are currently being investigated) and bariatric surgery for obesity during adolescence will increase the proportion of adolescents who reach and maintain reduced BMIs is unknown, given the substantial weight regain that occurs when antiobesity medications are discontinued for any reason. Lifelong treatment of obesity is needed but is burdensome and cost-prohibitive, with disparities in access. Long-term data regarding treatment effectiveness and safety, including mental health outcomes, are needed to determine cost–benefit ratios. More attention to public health interventions (e.g., policies to discourage sugar-sweetened beverages) and community strategies (e.g., infrastructure for safe, healthy environments and community coalitions) is needed to reduce obesity in children and adolescents.
Guidelines
Consensus recommendations for the assessment, treatment, and prevention of obesity are endorsed by the Pediatric Endocrine Society and the European Society of Endocrinology.22 The American Academy of Pediatrics recently published clinical practice guidelines that highlight the urgency of providing obesity treatment (≥26 hours of consultation for health behavior and lifestyle changes, with consideration of antiobesity medications as indicated) to each patient as soon as the diagnosis of obesity is made.18 Our recommendations are consistent with these guidelines, with the acknowledgment that the costs and limited access to these therapies and the inadequacy of long-term outcomes data for medication use are major barriers.
Conclusions and Recommendations
The patient described in the vignette has severe obesity that started at 6 years of age and in the ensuing 6 years progressed to include coexisting conditions such as prediabetes, dyslipidemia, and nonalcoholic fatty liver disease. Had we seen him at 6 years of age, we would have recommended intensive lifestyle intervention; to date, there are no approved antiobesity medications for children younger than 12 years of age. At this time, we would recommend intensive lifestyle intervention together with an antiobesity medication selected according to patient preference and weight-loss effect; currently, a GLP-1 receptor agonist would be the medication of choice given the effectiveness of these agents in clinical trials and the ease of administration. He should have follow-up visits every 3 months for surveillance of BMI and assessment of conditions associated with obesity and should receive treatment as needed. If surgical intervention is indicated in the future, he should be informed of the option for referral for evaluation for bariatric surgery at a comprehensive multidisciplinary pediatric center.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
Author Affiliations
From the Department of Pediatrics, Division of Pediatric Endocrinology and Diabetology, Indiana University School of Medicine, Indianapolis (T.S.H.); and the Center for Pediatric Research in Obesity and Metabolism and the Division of Pediatric Endocrinology, Metabolism, and Diabetes Mellitus, UPMC Children’s Hospital of Pittsburgh, Pittsburgh (S.A.A.).
Dr. Arslanian can be contacted at silva.arslanian@chp.edu or at the Division of Pediatric Endocrinology, Diabetes, and Metabolism, University of Pittsburgh, School of Medicine, UPMC Children’s Hospital of Pittsburgh, 4401 Penn Ave., FOB 6th Fl., Pittsburgh, PA 15224.
References
1. Twig G, Zucker I, Afek A, et al. Adolescent obesity and early-onset type 2 diabetes. Diabetes Care 2020; 43:1487-1495.
2. Vos MB, Abrams SH, Barlow SE, et al. NASPGHAN clinical practice guideline for the diagnosis and treatment of nonalcoholic fatty liver disease in children: recommendations from the Expert Committee on NAFLD (ECON) and the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition (NASPGHAN). J Pediatr Gastroenterol Nutr 2017;64:319-334.
3. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents, National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics 2011; 128:Suppl 5:S213-S256.
4. Ibáñez L, Oberfield SE, Witchel S, et al. An international consortium update: pathophysiology, diagnosis, and treatment of polycystic ovarian syndrome in adolescence. Horm Res Paediatr 2017;88:371-395.
5. Wise MS, Nichols CD, Grigg-Damberger MM, et al. Executive summary of respiratory indications for polysomnography in children: an evidence-based review. Sleep 2011;34(3): 389-398AW.
6. Puhl RM, Lessard LM. Weight stigma in youth: prevalence, consequences, and considerations for clinical practice. Curr Obes Rep 2020;9:402 -411.
7. Baker JL, Olsen LW, Sørensen TI. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med 2007;357: 2329-2337.
8. Twig G, Yaniv G, Levine H, et al. Body-mass index in 2.3 million adolescents and cardiovascular death in adulthood. N Engl J Med 2016;374:2430-2440.
9. Lindberg L, Danielsson P, Persson M, Marcus C, Hagman E. Association of childhood obesity with risk of early all-cause and cause-specific mortality: a Swedish prospective cohort study. PLoS Med 2020;17(3):e1003078-e1003078.
10. Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med 2011;365:1 876-1885.
11. Anekwe CV, Jarrell AR, Townsend MJ, Gaudier GI, Hiserodt JM, Stanford FC. Socioeconomics of obesity. Curr Obes Rep 2020;9:272-279.
12. Boyland EJ, Nolan S, Kelly B, et al. Advertising as a cue to consume: a systematic review and meta-analysis of the effects of acute exposure to unhealthy food and nonalcoholic beverage advertising on intake in children and adults. Am J Clin Nutr 2016;103:519-533.
13. Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA 2018;319:1723-1725.
14. Woolford SJ, Sidell M, Li X, et al. Changes in body mass index among children and adolescents during the COVID-19 pandemic. JAMA 2021;326: 1434-1436.
15. McCormick DW, Richardson LC, Young PR, et al. Deaths in children and adolescents associated with COVID-19 and MIS-C in the United States. Pediatrics 2021;148(5): e20210522 73-e2021052273.
16. Hales CM, Freedman DS, Akinbami L, Wei R, Ogden CL. Evaluation of alternative body mass index (BMI) metrics to monitor weight status in children and adolescents with extremely high BMI using CDC BMI-for-age growth charts. Vital Health Stat 1 2022;(197): 1-42.
17. Wolf RM, Nagpal M, Magge SN. Diabetes and cardiometabolic risk in South Asian youth: a review. Pediatr Diabetes 2021;22:52-66.
18. Hampl SE, Hassink SG, Skinner AC, et al. Clinical practice guideline for the evaluation and treatment of children and adolescents with obesity. Pediatrics 2023;151(2): e2022060 640-e2022060640.
19. Merrick MT, Ford DC, Ports KA, et al. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention — 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019;68:999-1005.
20. Malhotra S, Sivasubramanian R, Srivastava G. Evaluation and management of early onset genetic obesity in childhood. J Pediatr Genet 2021;10:194-204.
21. Flynn JT, Kaelber DC, Baker-Smith CM, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 2017;140 (3): e20171904-e20171904.
22. Styne DM, Arslanian SA, Connor EL, et al. Pediatric obesity-assessment, treatment, and prevention: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2017;102:709-757.
23. ElSayed NA, Aleppo G, Aroda VR, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes — 2023. Diabetes Care 2023;46:Suppl 1:S19-S40.
24. International Expert Committee. International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 2009;32:1327-1334.
25. Lee JM, Wu E-L, Tarini B, Herman WH, Yoon E. Diagnosis of diabetes using hemoglobin A1c: Should recommendations in adults be extrapolated to adolescents? J Pediatr 2011;158(6):947-952.e3.
26. Chaput JP, Willumsen J, Bull F, et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Act 2020;17: 141-141.
27. Vallabhan MK, Jimenez EY, Nash JL, et al. Motivational interviewing to treat adolescents with obesity: a meta-analysis. Pediatrics 2018;142 (5):e20 180733-e20180733.
28. Grossman DC, Bibbins-Domingo K, Curry SJ, et al. Screening for obesity in children and adolescents: US Preventive Services Task Force recommendation statement. JAMA 2017;317:2417-2426.
29. Muth ND, Dietz WH, Magge SN, et al. Public policies to reduce sugary drink consumption in children and adolescents. Pediatrics 2019;143 (4):e20190282-e20190282.
30. Nguyen M, Jarvis SE, Tinajero MG, et al. Sugar-sweetened beverage consumption and weight gain in children and adults: a systematic review and meta-analysis of prospective cohort studies and randomized controlled trials. Am J Clin Nutr 2023;117:160-174.
31. Pauley M, Mays C, Bailes JR Jr, et al. Carbohydrate-restricted diet: a successful strategy for short-term management in youth with severe obesity — an observational study. Metab Syndr Relat Disord 2021;19: 281-287.
32. Andela S, Burrows TL, Baur LA, Coyle DH, Collins CE, Gow ML. Efficacy of very low-energy diet programs for weight loss: a systematic review with meta-analysis of intervention studies in children and adolescents with obesity. Obes Rev 2019;20: 871-882.
33. House ET, Gow ML, Lister NB, et al. Pediatric weight management, dietary restraint, dieting, and eating disorder risk: a systematic review. Nutr Rev 2021;79:1114-1133.
34. Alman KL, Lister NB, Garnett SP, Gow ML, Aldwell K, Jebeile H. Dietetic management of obesity and severe obesity in children and adolescents: a scoping review of guidelines. Obes Rev 2021;22(1): e13132-e13132.
35. Kelley GA, Kelley KS, Pate RR. Exercise and adiposity in overweight and obese children and adolescents: a systematic review with network meta-analysis of randomised trials. BMJ Open 2019;9(11):e031220-e031220.
36. Lee S, Bacha F, Hannon T, Kuk JL, Boesch C, Arslanian S. Effects of aerobic versus resistance exercise without caloric restriction on abdominal fat, intrahepatic lipid, and insulin sensitivity in obese adolescent boys: a randomized, controlled trial. Diabetes 2012;61: 2787-2795.
37. Al-Khudairy L, Loveman E, Colquitt JL, et al. Diet, physical activity, and behavioral interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev 2017;6 (6): CD012691-CD012691.
38. Kelly AS, Auerbach P, Barrientos-Perez M, et al. A randomized, controlled trial of liraglutide for adolescents with obesity. N Engl J Med 2020;382: 2117-2128.
39. Weghuber D, Barrett T, Barrientos-Pérez M, et al. Once-weekly semaglutide in adolescents with obesity. N Engl J Med 2022;387: 2245-2257.
40. Hsia DS, Gosselin NH, Williams J, et al. A randomized, double-blind, placebo-controlled, pharmacokinetic and pharmacodynamic study of a fixed-dose combination of phentermine/topiramate in adolescents with obesity. Diabetes Obes Metab 2020;22:480-491.
41. Mead E, Atkinson G, Richter B, et al. Drug interventions for the treatment of obesity in children and adolescents. Cochrane Database Syst Rev 2016; 11:CD012436-CD012436.
42. Dhillon S. Phentermine/topiramate: pediatric first approval. Paediatr Drugs 2022;24:715-720.
43. Sadeghi A, Mousavi SM, Mokhtari T, Parohan M, Milajerdi A. Metformin therapy reduces obesity indices in children and adolescents: a systematic review and meta-analysis of randomized clinical trials. Child Obes 2020;16:174-191.
44. Inge TH, Courcoulas AP, Jenkins TM, et al. Five-year outcomes of gastric bypass in adolescents as compared with adults. N Engl J Med 2019;380: 2136-2145.
45. Järvholm K, Janson A, Peltonen M, et al. Metabolic and bariatric surgery versus intensive non-surgical treatment for adolescents with severe obesity (AMOS2): a multicentre, randomised, controlled trial in Sweden. Lancet Child Adolesc Health 2023;7:249-260.
46. White GE, Boles RE, Courcoulas AP, et al. A prospective cohort of alcohol use and alcohol-related problems before and after metabolic and bariatric surgery in adolescents. Ann Surg 2022 November 17 (Epub ahead of print).
47. Fennig U, Snir A, Halifa-Kurzman I, Sela A, Hadas A, Fennig S. Pre-surgical weight loss predicts post-surgical weight loss trajectories in adolescents enrolled in a bariatric program. Obes Surg 2019;29:1154-1163.
CREDIT: Hannon TS, Arslanian SA. Obesity in Adolescents. N Engl J Med. 2023 Jul 20;389(3):251-261. doi:10.10 56/NEJMcp2102062. PMID: 37467499.