Aleksander Zwierz, MD, PhD1, Krystyna Masna, MD1, Paweł Burduk, MD, PhD1
1Faculty of Health Sciences, Department of Otolaryngology, Oncology and Oral and Maxillofacial Surgery, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University, Bydgoszcz, Poland
Corresponding Author: Aleksander Zwierz, Faculty of Health Sciences, Department of Otolaryngology, Oncology and Oral and Maxillofacial Surgery, Collegium Medicum in Bydgoszcz, Nicolaus Copernicus University, Bydgoszcz, Poland.
Email: aleksanderzwierz@gmail.com
Abstract
The aim of this article was to feature the use of giant bilobed flaps in surgical reconstruction after total or subtotal petrosectomy in oncology cases. The Esser technique was renewed and adopted for coverage of huge skin loss. The authors reported 4 cases illustrated pre-and postoperative photography and intraoperative planning and schema. Good coverage and healing with no need for use of free tissue transfer or skin expanders or skin grafts were obtained. In the authors’ opinion, the cosmetic effect was acceptable. Surgical times of operation were significantly shorter.
Keywords ear cancer, SCC of the ear, petrosectomy, bilobed flaps, regional flaps in ear reconstruction
Introduction
Huge ear cancers are difficult for resection because of a lack of right margin of excision and trouble for covering the defect. Usually, we perform lateral or subtotal petrosectomy with parotidectomy and auricular resection. Because of the limitation of skin and poor mobility, free skin grafts, free flaps, pedicle flaps, or large local rotational flaps should be used. In our experience, the giant bilobed rotational flap is sufficient.
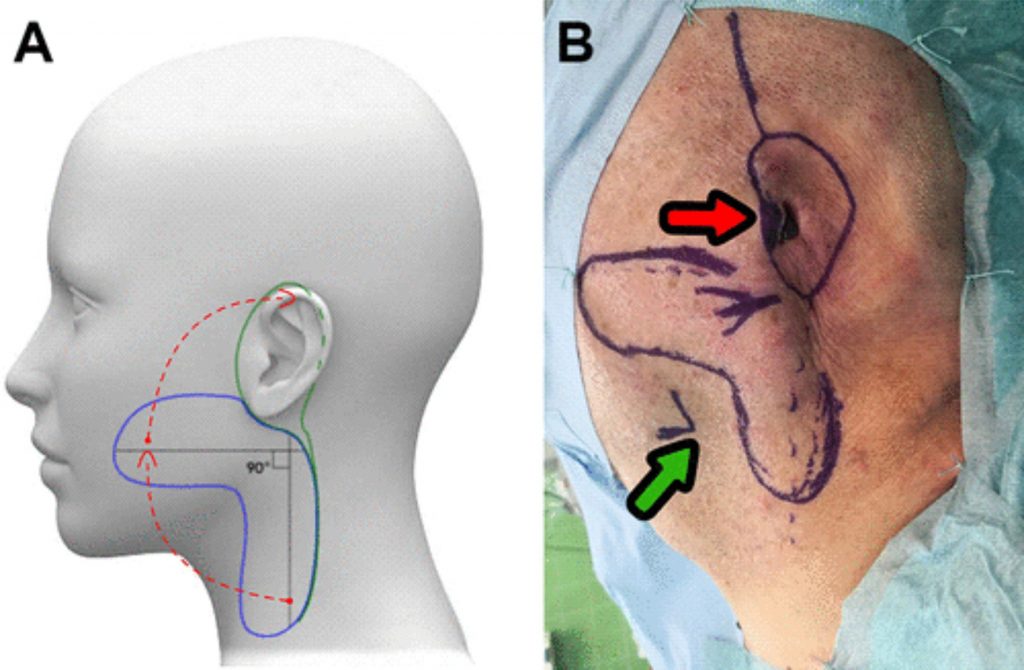
The bilobed flap was initially introduced for skin defects reconstruction after cancer of the nose resection. It is a double transposition flap described by Esser in 1918 and modified by Zitelli in 1989.1,2 The difference is in the angle between the 2 created flaps, 45° instead of 90°. We presented cases in which we used a giant bilobed flap for skin coverage and temporalis muscle rotation for reconstruction defects after petrosectomy.
Materials and Methods
We presented 4 cases of patients who had gone through subtotal petrosectomy because of the middle ear and external ear cancer. Histologically in 3 cases, it was squamous cell carcinoma (SCC) and in one it was melanoma. In 3 cases, we operated on patients with cancer recurrence, originally operated on in other centres.
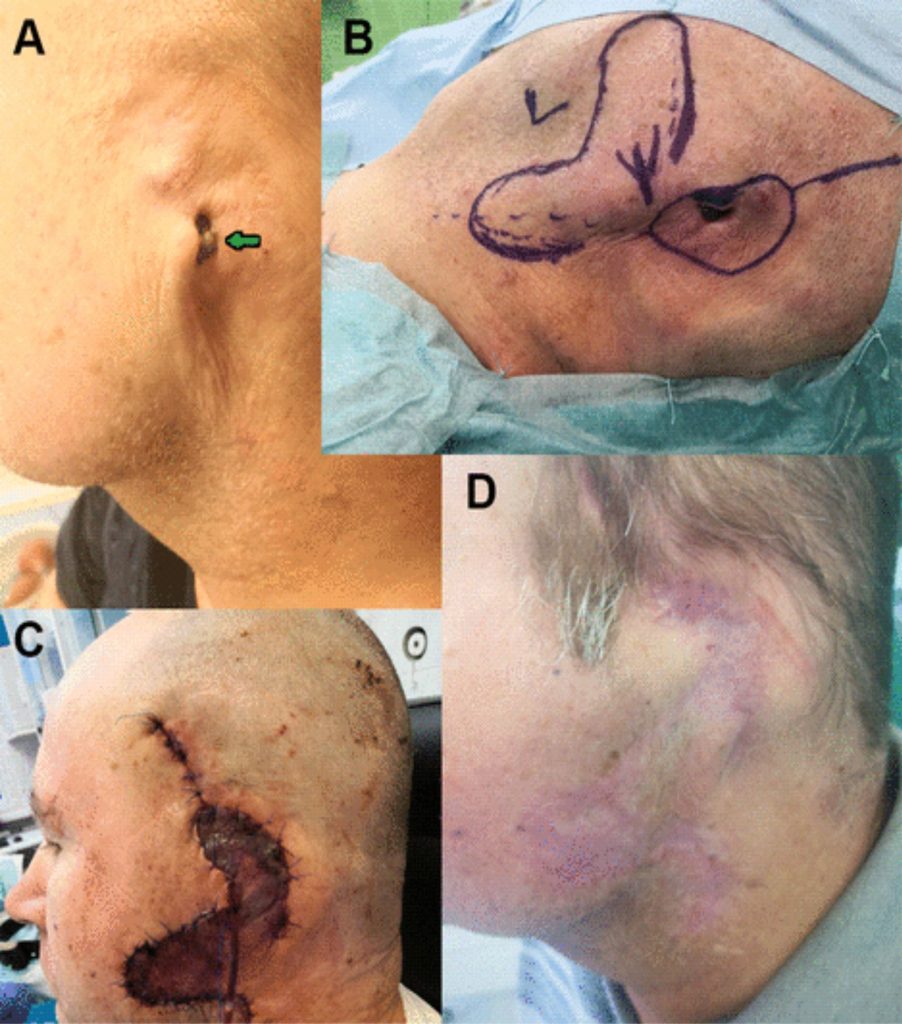
The first case is 80-year-old man, having squamous cell carcinoma of the left ear pinna and back wall of the external auditory canal. This patient was admitted and reoperated because of recidivism after subtotal auricular resection. Under general anaesthesia, we mentioned total auricular resection, tissue defect was oval-shaped 5 × 3 cm and was covered with rotated bilobed skin flaps. The patient has been discharged from the hospital in good condition. He was not postoperatively irradiated. We present our results after 6 months (Figure 1).
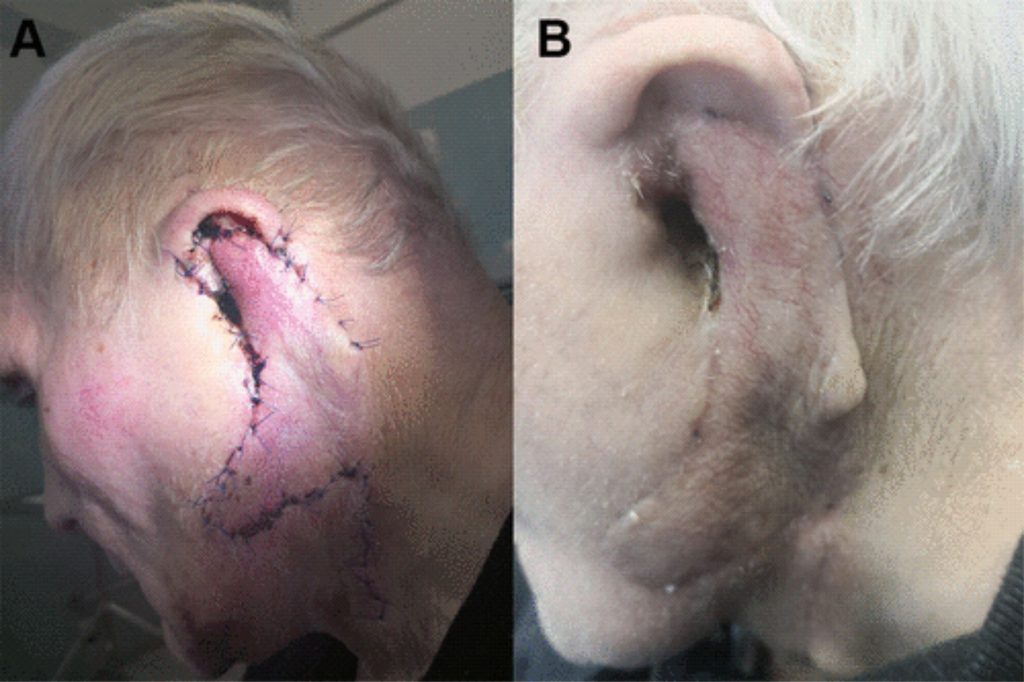
The next case of the flap was used for reoperation because of external auditory canal melanoma recurrence after the total auricular resection and complementary chemotherapy. In 2016, the patient underwent a metastatic lung tumour operation. Three years later, a growing local lesion was noted, filling the left external auditory canal. Subtotal pectrosectomy and superficial parotidectomy were done with a bilobed flap to reconstruct the oval defect 4 × 6 cm in size with a good esthetic effect (Figure 2). The patient has outgone postoperative chemotherapy
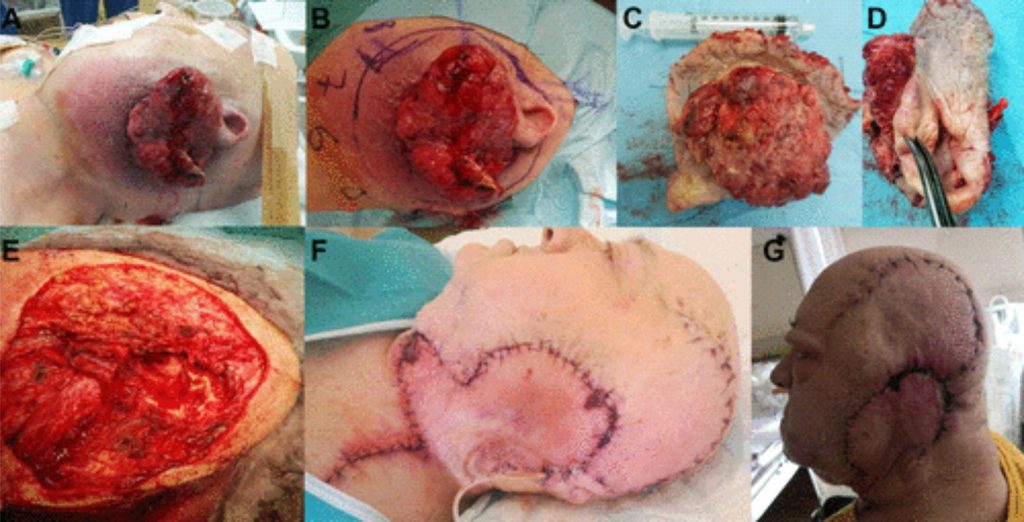
The third patient was hospitalized because of a large tumour coming out of the left external ear with infiltration of surrounding tissues. There were 2 attempts to remove the pathological mass in 2017 and 2018 but the recurrent occurred. In 2019, we performed a left-side petrosectomy with total parotidectomy and neck dissection. There was a huge circular skin defect, 17 cm in diameter. The post operated cavity was obliterated with temporalis muscle and overlaid it by the bilobed flap. Additionally, we mobilized the flap form the scalp to allow adequate skin loss coverage (Figure 3). Unfortunately, complementary radiotherapy was ceased, which contributes to early breakthrough disease.
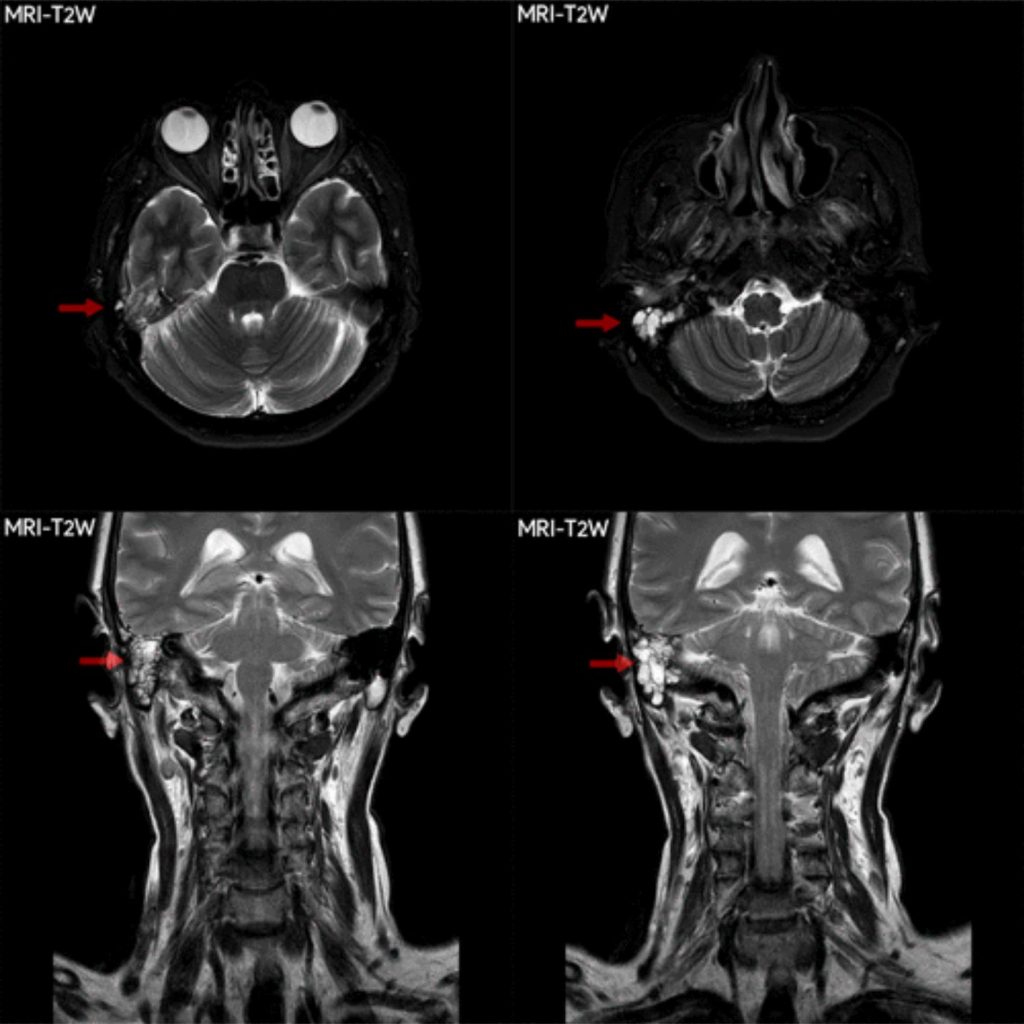
The fourth case was SCC of the middle ear with infiltration of temporomandibular joint and destruction of the temporal bone pyramid in the direction of the cerebral meninges (Figure 4).
Subtotal auricular resection and subtotal pertosectomy were performed with lateral parotidectomy and described reconstruction technic (Figure 5). The bilobed flap covered 4 × 6 cm oval-shaped skin defect. This patient has outgone postoperative radiotherapy.

Surgical Technique
We performed total or subtotal auricular resection, lateral or subtotal petrosectomy with total, partial or lateral parotidectomy and neck dissection. In all cases of petrosectomy, we use temporal muscle to fill to obliterate the cavity and coverage with bilobed flap from cheek and neck according to the Esser technique. Two flaps consisted of skin and subcutaneous tissues were raised. One bigger from cheek and second 20% smaller from the neck were 90° rotated, the flap from cheek covered loss of skin tissue and the second covered the cheek (Figure 6). The skin of the neck was mobilized and on both sides sewn. There was no previous radiotherapy performed in all cases. We excluded such patients due to the high potential for venous congestion or skin dehiscence. Additionally, we didn’t qualify for this type of bilobed flap reconstruction men who underwent previous on the same side neck dissection because of skin scaring and poorer blood supply.
Discussion
Large cancer resection from the head is especially difficult due to extensive soft tissue resection, a problem with obtaining a proper margin of the resection without destruction of critical structures, large bony defects, and difficulty with the eke out tissue and coverage with the skin.3 The surgeon is faced with large tissue loss. The goal is to provide cutaneous wound closure. The possibility for skin fill up comes from rotational flaps transfer, pedicle flaps, or free flaps.4 Temporalis and sternocleidomastoid muscles are used for packing defects of the lateral skull base but they should be covered with free skin or rotational flaps. Pectoralis major myocutaneous flap and the supraclavicular island fasciocutaneous flap can be used as well. Free flaps types consist of the rectus abdominis, transverse rectus abdominis myocutaneous, latissimus dorsi, anterolateral thigh (ALT)—most suitable, fibula osteocutaneous, radial forearm fasciocutaneous, radial forearm osteocutaneous, and gracilis are a good treatment of choice but difficult to perform and time-consuming.4,5 Some of the authors suggest using free flaps for reoperations if the other methods are unavailable.5-7 In our cases, skin transfer from the neck and cheek is the way to supply the lack of tissue.
Additionally, usage of temporalis muscle with saved posterior temporalis artery branch, as a base surface supporting the graft seems to be advantageous for blood supply for the skin flap then usage other tissue like the free fat from the abdomen.8 Temporalis muscle flap got better blood supply then sternocleidomastoideus flap especially if there is neck dissection performed which scarifies small blood supplying vessels. It should be stated that in the case of the patients with late-stage diseases, more aggressive operations should be considered and its favourable surgery then radiotherapy, which eventually may be considered as adjuvant treatment.9
Conclusion
We use temporalis muscle in our clinic, for post-resection cavity obliteration and covered with large bilobed flap proposed by Esser. We obtain good coverage and healing (Figure 5). The skin rotation and folding form a structure similar to ear lobe with good cosmetic results. Surgical times of operation were significantly shorter. We recommend this method especially for the elderly individual and serious conditions patients who weren’t previously irradiated or had no neck dissection surgery.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Aleksander Zwierz
https://orcid.org/0000-0002-5824- 8709
References
1. Baird, BJ, Moubayed, SP, Most, SP. A comparison of the double-half bilobed flap to the traditional bilobed flap: a cohort analysis of a single surgeon experience. Facial Plast Surg. 2017;33(5):526–529. DOI: 10.1055/s-0037-1606333. Google Scholar | Crossref | Medline
2. Steiger, J.D. Bilobed flaps in nasal reconstruction. Facial Plast Surg Clin North Am. 2011;19(1):107 –111. doi:10.1016/j.fsc.2010.10. 013. Google Scholar | Crossref | Medline
3. Hanasono, M.M, Silva, A.K, Yu, P, Skoracki, RJ, Sturgis, EM, Gidley, PW. Comprehensive management of temporal bone defects after oncologic resection. Laryngoscope. 2012; 122(12):2663–2669. doi:10. 1002/lary. 23528. Google Scholar | Crossref | Medline
4. Patel, NS, Modest, MC, Brobst, TD, Carlson, ML, Price, DL, Moore, EJ, Janus, JR. Surgical management of lateral skull base defects. Laryngoscope. 2016;126(8):1911 – 1917. https://doi.org/10.1002 /lary.25717. Google Scholar
5. Wehage, IC, Fansa, H. Complex reconstructions in head and neck cancer surgery: decision making. Head Neck Oncol. 2011;3:14. doi:10. 1186/1758-3284-3-14. Google Scholar | Crossref | Medline
6. Mourad, M, Arnaoutakis, D, Sawhney, R, Chan, D, Ducic, Y. Use of a giant bilobed flap for advanced head and neck defects. Facial Plast Surg. 2016;32(3):320–324. doi:10.1055/ s-0036-1571808. Google Scholar | Crossref | Medline
7. Arpa, SD, Cordova, A, Moschella, F. Further application of the bilobed flap: the split bilobed flap for reconstruction of composite posterior auricular and mastoid defects. J Plast Reconstr Aesthet Surg. 2006;59(12): 1330–1335. doi:10.1016/j.bjps. 2006.06.022. Google Scholar | Crossref | Medline
8. Hwang, E, Kim, YS, Chung, S. A new skin flap method for total auricular reconstruction in microtia patients with a reconstructed ear canal: extended scalp and extended mastoid postauricular skin flaps. J Plast Reconstr Aesthet Surg. 2014;67(6):770–774. doi:10. 1016/j.bjps.2014.02.012. Google Scholar |Crossref | Medline
9. Chang, CH, Shu, MT, Lee, JC, Leu, YS, Chen, YC, Lee, KS. Treatments and outcomes of malignant tumours of the external auditory canal. Am J Otolaryngol. 2009;30(1): 44–48. doi:10.1016/j. amjoto.2008.02.007. Epub 2008 Jul 22. Google Scholar | Crossref | MedlineView Abstract
Credits: Zwierz A, Masna K, Burduk P. The Use of Giant Bilobed Flaps for Tissue Defect Reconstruction After Temporal Bone and Ear Resection