Kamaluddin Latief, Samuel Akyirem, Siriluk Sithichoksakulchai, Dieta Nurrika, Mokh. Sujarwadi & Faizul Hasan
Abstract
Background
Sleep disturbance is common among people with hypertension. However, the mediating role of sleep disturbance in the association between hypertension and depression remains unclear. This study aims to investigate the mediating role of sleep disturbance in the association between hypertension and depression.
Materials and methods
This was a cross-sectional study. The data were derived from the Indonesian Family Life Survey Fifth Wave (2014–2015). We include a total of 19,138 adult participants with an age range from 18 to 65 years old who completed responses on the variable of hypertension, sleep disturbance, and depression. The mediating model analysis was processed using the PROCESS macro in SPSS from the Hayes model.
Results
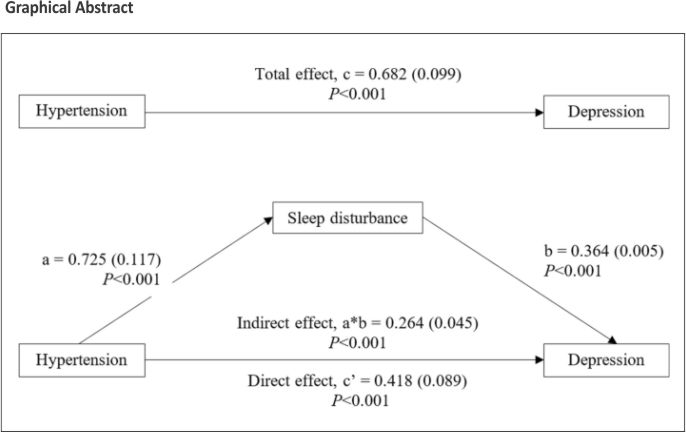
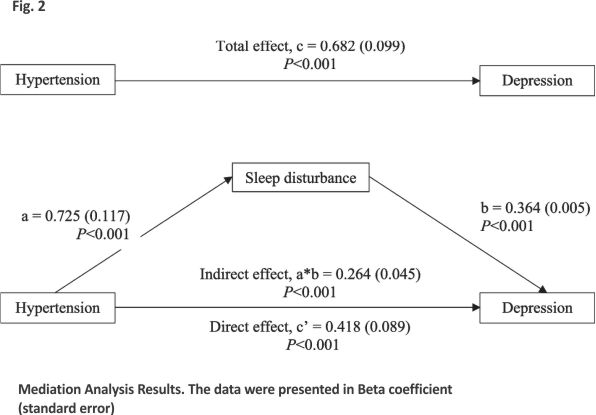
Depression was reported by 22% of total respondents. The group with hypertension showed a substantially higher prevalence of depression than non-hypertension group (P < 0.001). Hypertension had a significant overall effect on depression (β = 0.682; 95%CI 0.489 to 0.875, P < 0.001). The direct effect of hypertension on depression was significant (β = 0.418; 95%CI 0.244 to 0.592, P < 0.001) and the indirect effect mediated by sleep disturbance was also significant (β = 0.264, 95%CI 0.174 to 0.356, P < 0.001). It is worth noting that sleep disturbance partially mediated the association between hypertension and depression.
Conclusion
The findings of this study indicated that sleep disturbance contributed to the aetiology of depression and hypertension in adult populations. Nurses should be involved in managing sleep disturbances, such as using behavioural therapy, as it may serve as both a treatment and primary prevention measure for depression and hypertension.
Background
Hypertension is a common chronic condition with global prevalence ranging from 31 to 56% 1,2. In Indonesia, about 8.4% of adults have been diagnosed with hypertension by a medical doctor 3. Hypertension has been linked to elevated risk of cardiovascular comorbidities including stroke 4 and chronic kidney diseases 5,6. Other evidence suggests that people with hypertension are more likely to experience depression 7, 8.
Several studies have reported prevalence rates ranging from 22 to 32% 7,9. Previous studies suggest a bidirectional association between hypertension and depression 9,10. Depression may increase the risk of hypertension by activating the body’s stress responses and increasing autonomic nervous system activation 11. On the other hand, hypertension may increase the risk for depression by causing cerebrovascular pathologies 12 and increasing the sense of hopelessness related to living with a chronic condition 13. People who suffer from both depression and hypertension often report low quality of life 14. In addition, they usually experience sleep disturbances 15. While the underlying mechanism of the hypertension-depression relationship remains complex, sleep disturbance has been identified as a potential mediator 15.
Sleep disturbance has been linked to physical and mental health including cardiovascular disease and mood disorders 16. People with sleep problems have a high risk of developing hypertension 17 and depression 18. However, there is a lack of studies investigating the mediating role of sleep disturbance in the association between hypertension and depression. Hence, in this study, we aim to explore the mediating role of sleep disturbance in the association between hypertension and depression using nationally representative data from Indonesia.
Materials and methods
Data source and participants
The data was derived from the Indonesian Family Life Survey (IFLS) fifth Wave (IFLS-5), a cross-sectional study, fielded from September 2014 to April 2015. The IFLS sample represents approximately 83% of the Indonesian population living in 13 of the country’s 26 provinces, covering 16,204 households and 50,148 individuals 19. The IFLS has been conducted 5 times, in 1993, 1997, 2000, 2007, and 2014. The details of the study design of the IFLS-5 have been previously described 19. In this study, we include a total of 19,138 adult participants with ages ranging from 18 to 65 years old who have completed responses on the variables of hypertension, sleep disturbance, and depression.
Ethical approval
The IFLS data are accessible to the general public. Institutional review boards at the University of Gajah Mada in Indonesia and the RAND Corporation in the United States have examined and approved the survey’s methods with ethical clearance No.s0064-06-01-CR01 19. Before data collection began, all participants provided their written, informed consent.
Measurements
Depression
Depression was measured using the short-form Centres for Epidemiologic Studies Depression Scale (CES-D-10) 20. CES-D-10 consist of 10 items rated on a 4-point Likert scale ranging from 0 (rarely or none of the time) to 3 (all of the time) with a higher score indicating more depressive symptoms. A total score of 10 or higher is indicative of having depression. Previous studies revealed that this scale has acceptable validity and reliability 19.
Hypertension
Previous studies using IFLS data indicate that hypertension, as measured by blood pressure, covers approximately 40% of participants 21,22, while hypertension using self-reported measurements covers around 80% of participants 21. Therefore, in this study, hypertension was assessed using self-report, measured with the question, “Has a doctor, paramedic, or nurse ever told you that you had hypertension?”.
Sleep disturbance
Sleep disturbance was measured using the combination of five items of Patient-Reported Outcomes Measurement Information System (PROMIS) sleep disturbance measure 23 and five items of PROMIS sleep impairment measure 24. A previous study reported that the scale has a good Cronbach’s alpha of 0.82 25. Higher scores on the scales indicate more sleep disturbance with a cut-off point of 11 or higher indicating having sleep disturbance 25.
Lifestyle and comorbidity condition
Smoking status was measured and classified into three groups (never, quitters and current tobacco users) 19. Physical activity was measured using the short version of the International Physical Activity Questionnaire (IPAQ) for the last 7 days (IPAQ-S7S) 26. It is divided into three levels low, moderate, and high intensity physical activity. Additionally, outpatient care was assessed using a single-item questionnaire 19. For comorbidity conditions (diabetes mellitus, tuberculosis, asthma, lung condition, heart attack, liver disease, stroke, cancer, high cholesterol, kidney disease, stomach or other digestive disease, and psychiatric problem). It was measured using single-item questions such as ‘Has a doctor/paramedic/nurse/midwife ever told you that you had…? to which participants answered “yes” or “no” 19.
Demographic
In addition, demographic variables including age, gender, marital status, attending school, and education level were added in this study 19.
Statistical analyses
In the beginning, we used STATA software for all data processing. In the second stage, we used SPSS software version 29.0 to perform all statistical analyses (IBM, Armonk, NY, USA). A two-tailed P < 0.05 was considered as a statistically significant level. To analyse the differences in the baseline characteristics between the 2 groups, we used the chi-squared or Fisher’s exact test for categorical variables and independent t-tests for continuous variables. The correlation between the main variables (hypertension, sleep disturbance, and depression) was measured using Pearson and Spearman correlation. Univariate and multivariate linear regression analyses were also performed. Finally, the mediating model analysis was processed using the PROCESS macro in SPSS from Hayes model 27.
Result
Study characteristic
Figure 1 depicts the participants’ flow diagram. In total, there were 25,824 adult participants were screened for eligibility. Of these, a total of 6,686 participants were excluded, with 779 not responding to questionnaires and 5,907 having missing data. This included missing data in the ‘hypertension’ variable (n = 4,932), ‘depression’ variable (n = 966), and ‘sleep disturbance’ variable (n = 9). Finally, a total of 19,138 participants were included in the main analysis. Hypertension was confirmed for 2,736 (14.3%) individuals.

Demographic comparisons between patients with hypertension (n = 2,736) and those without hypertension (n = 16,402) were presented in Table 1. The prevalence of hypertension varies across age groups, with rates of 6.5% for the 18–34 age group, 13.1% for the 35–49 age group, and 25.9% for the 50–65 age group. Most of the participants were married (84%) and 96% of them attended the school.
The comparison of lifestyle and comorbidity conditions is presented in Table 2. In total 37% of included participants were smokers. The hypertension group had higher sleep disturbance compared to the non-hypertension group. There is a significant difference between the two groups in terms of physical activity (vigorous and low activity levels) (P < 0.001 and P = 0.001, respectively). Other details of the variable can be seen in Table 2.
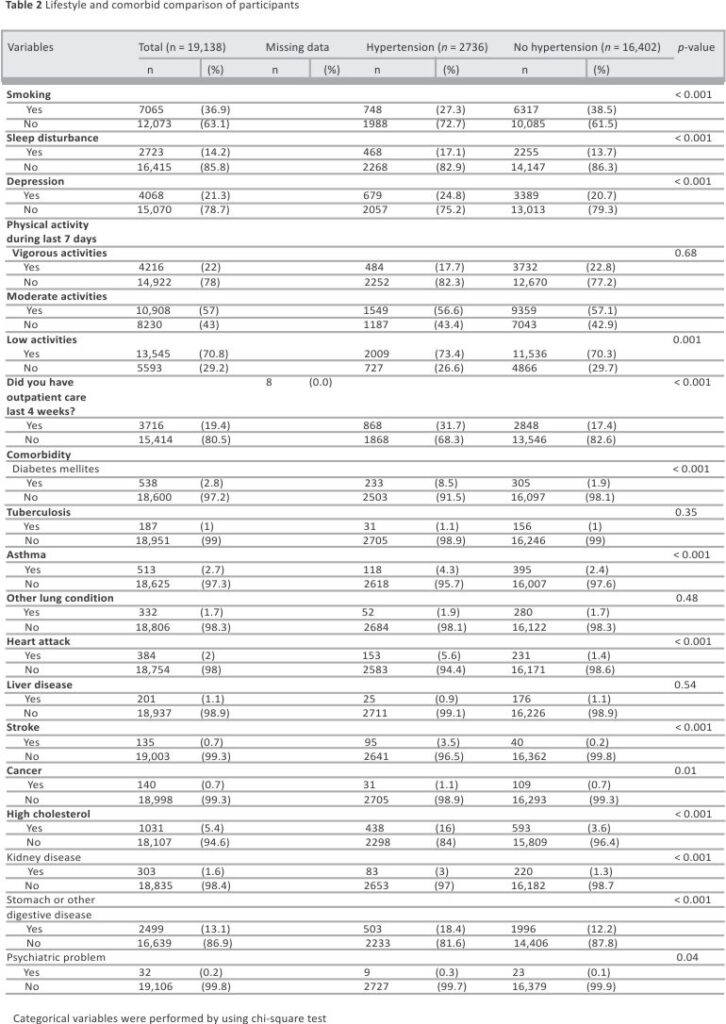
Depression
Depression was reported in 22% of the total sample. The group with hypertension had a significantly higher depression prevalence compared to the non-hypertension group (see Table 2, P < 0.001). Supplementary Table S1 presented the responses of participants who endorsed each of the depression questionnaires.
Association between hypertension, sleep disturbance, and depression
Supplementary Table S2 shows the association between hypertension, sleep disturbance, and depression. The hypertension variable had a significant positive correlation with depression (r = 0.05, P < 0.001). The hypertension variable also has a significant positive correlation with sleep disturbance (r = 0.05, P < 0.001). Similarly sleep disturbance variable also has a significant positive correlation with depression (r = 0.44, P < 0.001).
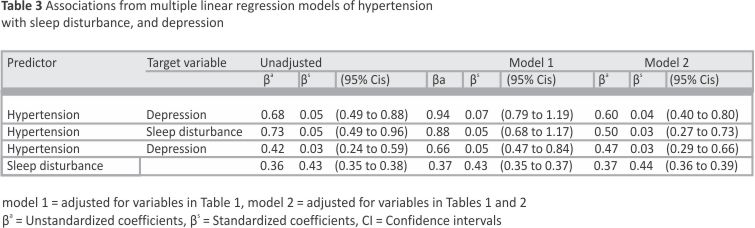
The bivariate and multiple linear regression results are displayed in Table 3. In the unadjusted model, all predictors show a significant positive association with the target variable. When hypertension and sleep disturbance are combined as predictors in Model 1, the association remains significantly positive. In Model 2, all predictors also exhibit a significant positive association with the outcome variables.
The mediating effect of sleep disturbance on the association between hypertension and depression
The simple mediating analysis indicated that sleep disturbance partially mediated the association between hypertension and depression. As shown in Fig. 2 and Supplementary Table 3, hypertension was positively associated with sleep disturbance (a = 0.725), and sleep disturbance was positively associated with depression (b = 0. 364). Based on 5,000 bootstrap resamples, the bootstrap confidence interval for the indirect effect (ab = 0.264) was entirely above zero, ranging from 0.174 to 0.356. The total effect of hypertension on depression was significant (β = 0.682; 95% CI 0.489 to 0.875, P < 0.001), comprising a direct effect (β = 0.418; 95% CI 0.244 to 0.592, P < 0.001) and an indirect effect (β = 0.264; 95% CI 0.174 to 0.356, P < 0.001).
Discussion
To the best of our knowledge, this is the first study investigating the mediating effect of sleep disturbance in the association between hypertension and depression. This study highlights that sleep disturbance becomes partial mediation in the association between hypertension and depression. Because the methodology is rigorous and we use a big sample size, hence our study should be considered.
Although the pathological mechanism of sleep disturbance after hypertension was complex. However, it can develop as a result of hypertension due to factors such as persistent physiological stress 28, increased sympathetic nervous system activity causing alertness 29,30, disrupted nighttime blood pressure patterns 31, potential sleep-affecting medication side effects 32, psychological impact from hypertension management 33, and endothelial dysfunction 34,35, all of which contribute to sleep disruptions. Effective hypertension treatment, lifestyle changes 36, and stress reduction measures are critical for sleep disturbance 37. If sleep problems persist, it is critical to consult a healthcare practitioner, as treating hypertension may improve sleep quality 37,38,39.
In this study, sleep disturbance is observed in approximately 17% of the hypertension group and 13.7% of the non-hypertension group. Consistent with previous studies, sleep disturbances such as obstructive sleep apnea (OSA) and insomnia are prevalent following hypertension 32,40,41. Evidence suggests that OSA becomes a significant risk factor for hypertension 42. Numerous pathways, including endothelial impairment 43,44, oxidative stress 45,46, inflammation 47,48, and sympathetic activation 49,50, are generally acknowledged as ways in which OSA leads to the development of hypertension. Of note, this study reveals that sleep disturbance partially mediates the association between hypertension and depression. It indicates that targeting depression treatment after hypertension should also consider sleep disturbance. We found that the prevalence of depression following hypertension in our study is 25% which is higher than in the non-hypertension group (21%, see Table 2). In line with previous studies, the prevalence of depression ranged from 22 to 32% following hypertension 7,9 and 13–17% in the general population 51,52. Because the presence of depression affects the health-related quality of life 14. Hence, clinicians and researchers need to implement the best treatment approach for depression.
Strengths and limitations
To the best of our knowledge, this study possesses several strengths. First, this study was nationally representative of the data since the study population was taken from participants across Indonesia. Second, all interviewers for the IFLS were trained to understand the methodology and the content of the questionnaire.
This study highlights several limitations. First, the data related severity of hypertension, subtype, and type of medication is not available. Second, potential confounders could not obtain such use hypnotic used, dietary factors, and environmental factors, which may threaten the internal validity. Third, the data related to blood pressure and medication for hypertension is unable to be provided. Fourth, the data related to hypertension was self-reported, which may cause information bias.
Conclusion
The result of this study suggested that sleep disturbance plays a role in the etiology of hypertension and depression in adult populations. The management of sleep disturbance could potentially serve as treatment and primary prevention for depression in these populations. Behavioural therapy could be implemented to reduce sleep disturbance.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
IFLS: Indonesian Family Life Survey
CES-D-10: Centers for Epidemiologic Studies Depression Scale
PROMIS: Patient-Reported Outcomes Measurement Information System
IPAQ: International Physical Activity Questionnaire
OSA: Obstructive sleep apnea
References
1. Bloch MJ. The worldwide prevalence of hypertension exceeds 1.3 billion. J Am Soc Hypertens. 2016;10(10): 753–4.
2. Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004; 22(1):11–9.
3. Kemenkes RI. Laporan Nasional Riset Kesehatan Dasar. Kementerian Kesehatan RI. 2018. p. 203.
4. Wajngarten M, Silva GS. Hypertension and stroke: update on treatment. Eur Cardiol Rev. 2019;14(2):111.
5. Faraco G, Iadecola C. Hypertension: a harbinger of stroke and dementia. Hypertension. 2013;62(5):810 –7.
6. Lauder L, Mahfoud F, Azizi M, Bhatt DL, Ewen S, Kario K, et al. Hypertension management in patients with cardiovascular comorbidities. Eur Heart J. 2023; 44(23):2066–77.
7. Li Z, Li Y, Chen L, Chen P, Hu Y. Prevalence of depression in patients with hypertension: a systematic review and meta-analysis. Medicine. 2015;94: 31.
8. Villarreal-Zegarra D, Bernabe-Ortiz A. Association between arterial hypertension and depressive symptoms: results from population‐based surveys in Peru. Asia‐Pacific Psychiatry. 2020;12(2):e12385.
9. Mai AS, Lim OZH, Ho YJ, Kong G, Lim GEH, Ng CH, et al. Prevalence, risk factors and intervention for depression and anxiety in pulmonary hypertension: a systematic review and meta-analysis. Front Med. 2022;9: 765461.
10. Meng L, Chen D, Yang Y, Zheng Y, Hui R. Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies. J Hypertens. 2012;30(5):842–5 1.
11. Scalco AZ, Scalco MZ, Azul JBS, Neto FL. Hypertension and depression. Clinics. 2005;60(3) :241–50.
12. Turana Y, Tengkawan J, Chia YC, Shin J, Chen CH, Park S, et al. Mental health problems and hypertension in the elderly: a review from the HOPE Asia Network. J Clin Hypertens. 2021; 23(3):504–12.
13. Ang CW, Tan MM, Bärnighausen T, Reininghaus U, Reidpath D, Su TT. Mental distress along the cascade of care in managing hypertension. Sci Rep. 2022; 12(1): 15910.
14. Zhang Y, Zhou Z, Gao J, Wang D, Zhang Q, Zhou Z, et al. Health-related quality of life and its influencing factors for patients with hypertension: evidence from the urban and rural areas of Shaanxi Province, China. BMC Health Serv Res. 2016;16: 1–9.
15. Cai Y, Chen M, Zhai W, Wang C. Interaction between trouble sleeping and depression on hypertension in the NHANES 2005–2018. BMC Public Health. 2022;22(1):1–11.
16. Seow LSE, Tan XW, Chong SA, Vaingankar JA, Abdin E, Shafie S, et al. Independent and combined associations of sleep duration and sleep quality with common physical and mental disorders: results from a multi-ethnic population-based study. PLoS One. 2020;15(7):e02358 16.
17. Vgontzas AN, Liao D, Bixler EO, Chrousos GP, Vela-Bueno A. Insomnia with objective short sleep duration is associated with a high risk for hypertension. Sleep. 2009;32(4):491–7.
18. Kudlow P, Cha D, Lam R, McIntyre R. Sleep architecture variation: a mediator of metabolic disturbance in individuals with major depressive disorder. Sleep Med. 2013;14(10):943–9.
19. Strauss J, Witoelar F, Sikoki B. The fifth wave of the Indonesia family life survey: overview and field report, Vol. 1. Santa Monica: Rand; 2016. p. 1–94.
20. Knight RG, Williams S, McGee R, Olaman S. Psychometric properties of the Centre for epidemiologic studies depression scale (CES-D) in a sample of women in middle life. Behav Res Ther. 1997;35(4): 373–80.
21. Mahwati Y, Nurrika D, Latief K. The determinants of undiagnosed hypertension among Indonesian adults: a cross-sectional study based on the 2014–2015 Indonesia family life survey. J Prev Med Public Health. 2022;55(1):60.
22. Latief K, Nurrika D, Tsai M-K, Gao W. Body mass index Asian populations category and stroke and heart disease in the adult population: a longitudinal study of the Indonesia Family Life Survey (IFLS) 2007 and 2014. BMC Public Health. 2023;23(1): 2221.
23. Yu L, Buysse DJ, Germain A, Moul DE, Stover A, Dodds NE, et al. Development of short forms from the PROMIS™ sleep disturbance and sleep-related impairment item banks. Behav Sleep Med. 2012;10( 1): 6–24.
24. Buysse DJ, Yu L, Moul DE, Germain A, Stover A, Dodds NE, et al. Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010; 33(6):781–92.
25. Peltzer K, Pengpid S. Prevalence, social and health correlates of insomnia among persons 15 years and older in Indonesia. Psychol Health Med. 2019;24 (6):757–68.
26. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381– 95.
27. Hayes AF. Mediation, moderation, and conditional process analysis. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach, Vol. 1. 2013. p. 20.
28. Kalmbach DA, Cuamatzi-Castelan AS, Tonnu CV, Tran KM, Anderson JR, Roth T, et al. Hyperarousal and sleep reactivity in insomnia: current insights. Nat Sci Sleep. 2018;10:193–201.
29. Maes J, Verbraecken J, Willemen M, De Volder I, Van Gastel A, Michiels N, et al. Sleep misperception, EEG characteristics and autonomic nervous system activity in primary insomnia: a retrospective study on polysomnographic data. Int J Psychophysiol. 2014;91(3): 163–71.
30.Bonnet MH, Arand DL. Hyperarousal and insomnia: state of the science. Sleep Med Rev. 2010;14(1):9–15.
31. Maiolino G, Bisogni V, Soranna D, Pengo MF, Pucci G, Vettor R, et al. Effects of insomnia and restless legs syndrome on sleep arterial blood pressure: a systematic review and meta-analysis. Sleep Med Rev. 2021; 59: 101497.
32. Jarrin DC, Alvaro PK, Bouchard M-A, Jarrin SD, Drake CL, Morin CM. Insomnia and hypertension: a systematic review. Sleep Med Rev. 2018;41:3–38.
33. Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005; 111(5):697–716.
34. Portaluppi F, Tiseo R, Smolensky MH, Hermida RC, Ayala DE, Fabbian F. Circadian rhythms and cardiovascular health. Sleep Med Rev. 2012;16(2): 151–66.
35. Chen L, Yang G. Recent advances in circadian rhythms in the cardiovascular system. Front Pharmacol. 2015;6: 71.
36. Williams B, Poulter N, Brown M, Davis M, McInnes G, Potter J, et al. Guidelines for the management of hypertension: report of the fourth working party of the British Hypertension Society, 2004—BHS IV. J Hum Hypertens. 2004;18(3):139–8 5.
37. Lytle J, Mwatha C, Davis KK. Effect of lavender aromatherapy on vital signs and perceived quality of sleep in the intermediate care unit: a pilot study. Am J Crit Care. 2014;23 (1):24–9.
38. Carnethon MR, Johnson DA. Sleep and resistant hypertension. Curr Hypertens Rep. 2019;21:1–6.
39. Cho M-C. Clinical significance and therapeutic implication of nocturnal hypertension: the relationship between nighttime blood pressure and quality of sleep. Korean Circ J. 2019;49 (9):818–28.
40. Thomas SJ, Calhoun D. Sleep, insomnia, and hypertension: current findings and future directions. J Am Soc Hypertens. 2017;11(2): 122–9.
41. Pepin J-L, Borel A-L, Tamisier R, Baguet J-P, Levy P, Dauvilliers Y. Hypertension and sleep: overview of a tight relationship. Sleep Med Rev. 2014;18(6): 509–19.
42. Kareem O, Tanvir M, Naqash A, Bader GN. Obstructive sleep Apnoea: a risk factor for hypertension. J Cardiol Cardiovasc Sci. 2018;2(2): 20–8.
43. Hirata Y, Nagata D, Suzuki E, Nishimatsu H, Suzuki J-i, Nagai R. Diagnosis and treatment of endothelial dysfunction in cardiovascular disease a review. Int Heart J. 2010;51(1):1–6.
44. Jafari B, Mohsenin V. Endothelial dysfunction and hypertension in obstructive sleep apnea–Is it due to intermittent hypoxia? J Cardiovasc Disease Res. 2013; 4(2):87–91.
45. Lavie L. Oxidative stress in obstructive sleep apnea and intermittent hypoxia–revisited – the bad ugly and good: implications to the heart and brain. Sleep Med Rev. 2015; 20:27–45.
46. Eisele HJ, Markart P, Schulz R. Obstructive sleep apnea, oxidative stress, and cardio-vascular disease: evidence from human studies. Oxid Med Cell Longev. 2015;2015.
47. Unnikrishnan D, Jun J, Polotsky V. Inflammation in sleep apnea: an update. Rev Endocr Metab Disord. 2015;16:25–34.
48. Chul Sung K, Suh JY, Kim BS, Kang JH, Kim H, Lee MH, et al. High sensitivity C-reactive protein as an independent risk factor for essential hypertension. Am J Hypertens. 2003;16(6): 429–33.
49. Parati G, Lombardi C, Hedner J, Bonsignore MR, Grote L, Tkacova R, et al. Position paper on the management of patients with obstructive sleep apnea and hypertension: joint recommendations by the European Society of Hypertension, by the European Respiratory Society and by the members of European COST (Cooperation in Scientific and Technological Research) ACTION B26 on obstructive sleep apnea. J Hypertens. 2012;30(4):633–46.
50. Freet CS, Stoner JF, Tang X. Baroreflex and chemoreflex controls of sympathetic activity following intermittent hypoxia. Auton Neurosci. 2013;174 (1–2): 8–14.
51. Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci Rep. 2018;8(1):286 1.
52. Alamri HS, Algarni A, Shehata SF, Al Bshabshe A, Alshehri NN, ALAsiri AM, et al. Prevalence of depression, anxiety, and stress among the general population in Saudi Arabia during the Covid-19 pandemic. Int J Environ Res Public Health. 2020;17(24): 9183.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Global Health and Health Security, College of Public Health, Taipei Medical University, Taipei, Taiwan
Kamaluddin Latief
Centre for Family Welfare, Faculty of Public Health, Universitas Indonesia, Depok, Indonesia
Kamaluddin Latief
Yale School of Nursing, Yale University, New Haven, CT, USA
Samuel Akyirem
Department of Fundamental Nursing, Faculty of Nursing, Mahidol University, Bangkok, Thailand
Siriluk Sithichoksakulchai
College of Nursing, Kaohsiung Medical University, Kaohsiung, Taiwan
Siriluk Sithichoksakulchai
Public Health Study Program, Banten School of Health Science, South Tangerang, Indonesia
Dieta Nurrika
Culture, Research, and Technology, The Ministry of Education, Higher Education Service Institutions (LL-DIKTI) Region IV, Bandung, Indonesia
Dieta Nurrika
Faculty of Nursing, Universitas Jember, Jember, Indonesia
Mokh. Sujarwadi
Faculty of Nursing, Chulalongkorn University, Boromarajonani Srisataphat Building, 12th Floor Rama1 Road, Wang Mai, Pathum Wan, Bangkok, 10330, Thailand
Faizul Hasan
Contributions
FH and KL acquired data performed the statistical analyses, interpreted data, and drafted and revised the manuscript for important intellectual content and approved the final version. SA, SS, DN, and MS interpreted data, reviewed the analyses, and approved the final version.
Corresponding author
Correspondence to Faizul Hasan.
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Institutional review boards at the University of Gajah Mada in Indonesia and the RAND Corporation in the United States with ethical clearance No. s0064-06-01-CR01.
Consent for publication
Not applicable.
Competing interests
The authors declare no potential conflicts of interest.
Credits: Latief, K., Akyirem, S., Sithichoksakulchai, S. et al. The mediating effect of sleep disturbance on the association between hypertension and depression: a national data analysis. Clin Hypertens 30, 5 (2024). https://doi.org/ 10.1186/s40885-024-00263-y











