Adefunke DadeMatthews, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing, corresponding author 1,2,* Chukwuemeka
Nzeakah, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – original draft,# 2,3 Lucky Onofa, Conceptualization, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing – review & editing,# 2 Oluwagbemiga Dade Matthews, Funding acquisition, Methodology, Resources, Validation, Visualization, Writing – review & editing, 4, ‡ and Temitope Ogundare, Data curation, Methodology, Validation, Visualization, Writing – review & editing 5,
Lakshit Jain, Editor
Abstract
Background
Depressive disorders, with a prevalence of 15–21%, are among the most common disorders in children and adolescents, and increase the risk of suicide, the second leading cause of death in children aged 10 to 19.
Aim
To determine the prevalence and correlates of depressive disorders among senior students attending secondary schools in Abeokuta.
Method
The study was conducted in five schools randomly selected from a representative sample and was carried out in 2 phases. In the first phase, students were selected via systematic random sampling and given consent forms and GHQ-12 to administer to the parents. In the second phase, students who returned a signed informed consent form and filled out GHQ-12 were interviewed using MINI-KID, Rosenberg’s Self-Esteem Scale, Family-APGAR, and sociodemographic questionnaire. Multivariate regression analyses were conducted with a p-value <0.05 as a level of significance.
Results
The mean age was 15.3 years (SD = 1.27); 48.8% were male. The twelve-month prevalence of major depression was 11.3% and dysthymia was 1.4%. In the final regression analysis, female gender [OR = 4.3, p = 0.046], the experience of bullying [OR = 7.96, p = 0.004], difficulty getting along with friends, [OR = 7.5, p = 0.004], history of sexual abuse [OR = 8.1, p = 0.01], and perceived family dysfunction [OR = 4.9, p = 0,023] were found to be independent predictors of depressive disorders.
Conclusion
Depressive syndromes are a significant health burden in adolescents. Being female, being bullied, having a history of sexual abuse, and family dysfunctionality are risk factors associated with depression among these populations.
Introduction
Depressive disorders are among the most common disorders in children and adolescents, with a high prevalence of 12% 1 and rising to 21% 1–4. Depression increases the risk of suicide, the second leading cause of death in children and young adults between ages ten and twenty-four 5 and one of the top ten leading causes of death across all ages 5,6. The reported prevalence of depression among the adolescent population varies widely due to differences in the methodology of various epidemiological studies. Current literature suggests that major depressive disorder is more prevalent than dysthymia and other subtypes of depression 7,8. Before puberty, there is no significant difference in the prevalence of depression between the genders, but after that, an increased incidence in females is widely documented across various cultures 9,10. Overall, the prevalence of depression rises with an increasing number of adolescents ages 11–13.
Etiological models suggest that exposure to multiple antecedents interacts with innate characteristics to increase adolescents’ risk of depression. Individual risks for depression in adolescents include certain genetic factors, female gender, endocrine dysfunction, negative cognitive styles, sub-clinical depressive symptoms, specific personality traits, and problems in self-regulation/coping behaviours, while risks from the external environment include faulty parent-child relationships, adverse life events and on-going interpersonal difficulties 14–17.
The genetic contribution to the etiolog of adolescent depression appears to be moderate, with heritability estimates ranging between 40–70% 14,18. There is a three to four-fold increased risk of depression in the offspring of adults with unipolar depression compared to children of non-depressed parents 19, which is significantly higher in cases of post-natal maternal depression 20. This elevated risk is also seen in other forms of parental psycho-pathology, although the association’s strength is greatest for parental depression.
Studies have shown that low self-esteem, characterized by global self-devaluation, perceived incompetence, and negative attributional styles, are cognitive factors that markedly increase the risk of depression in adolescents 21,22. Furthermore, adolescents with a highly emotional temperamental style (neuroticism) characterized by reacting quickly to everyday events, being easily brought to tears, or easily soothed are also recognized to have a significantly elevated risk of depression 23.
Relational conflicts within the family environment play a major role in the etiology of adolescent depression. Studies show that insecure attachment and parenting characterized by coldness, rejection, harsh discipline, and unsupportive behaviour are associated with adolescent depressive symptoms 17. Parental psychopathology, particularly maternal depression, may contribute to chronic interpersonal stress in the family, compromising the quality of parenting, which may negatively affect youths’ psychosocial functioning 24. Other family-based pathogenic factors include physical abuse, neglect, absent monitoring, marital discord, low family cohesion, lack of authoritative parenting, severe acute disruptions such as sudden death or serious illness in a close relative and sudden parental separation 25–27.
Parental depressive symptoms, perception of poor family functioning, peer problems, low self-esteem, female gender, and large family size are some of the factors that have been associated with clinically significant depressive symptoms in adolescents 21. Other factors that are significantly associated with depression in adolescents include alcohol consumption, drug abuse 28, sexual activity 28,29, and physical violence 28–30. Lower levels of physical activity have also been linked with severe depressive symptoms 28, 31, while moderate physical activity was linked with reduced risk of depressive symptoms 28.
Depression is markedly increased due to multiple adverse experiences involving longstanding family and more recent friendship events and peer difficulties. Adolescents with poor friendships, characterized by low numbers of friends, infrequent contact, and no intimate relations, are more likely to develop depression, deviant behaviours, and increased social isolation from the desired peer network 22,32,33. Studies have also shown that adolescents who are bullied and those who are bullies are at an increased risk of depression and suicide 34,35.
Local studies on the prevalence and correlates of depression show findings largely comparable with results from elsewhere. A cross-sectional survey of adolescents in southwest Nigeria found that 5.1% met the criteria for a major depressive disorder (MDD) 4. A study using the Beck’s Depressive Inventory found 9% of school-attending adolescents in another southwestern town in Nigeria to have clinically significant depressive symptoms 21 with a diagnosis of MDD established in 6.9% of the total sample 36. In another cohort of high school students in a major city in north-eastern Nigeria, a 12% prevalence of depression was reported with 50% of the students who used substances reporting depression 2.
Several studies worldwide have sought to establish the prevalence and associated socioeconomic burden of depressive syndromes in adolescents. However, only a few studies have been done in Sub-Saharan Africa to address the subject 2,7,36–39. This study aims to determine the prevalence and correlates of depressive disorders among senior students attending secondary schools in Abeokuta.
Materials and methods
The study was carried out in Abeokuta, southwestern Nigeria. It is part of a larger study on anxiety and depressive disorders conducted among secondary school students aged 12–18 years, and the methodology has been described elsewhere 40. The study was conducted in 2 phases. In the first phase, students were selected via systematic random sampling and given consent forms and GHQ-12 to administer to the parents. In the second phase, students who returned a signed informed consent form and filled out GHQ-12 were interviewed using MINI-KID, Rosenberg’s Self-Esteem Scale, Family-APGAR, and sociodemographic questionnaire. Five schools were randomly selected, and from each school, a proportional sampling method, accounting for the sizes of each school, was employed. The sample size was calculated using the formula for estimating proportions 41.
Study instruments
Sociodemographic questionnaire This was designed to collect data on the sociodemographic characteristics of the participants and factors linked to depression, such as trauma exposure, history of medical illness, etc. It also collected information about family structure and health-related behaviours.
Rosenberg’s Self-Esteem Scale The 10-item Rosenberg’s Self-Esteem Scale 42 measures both positive and negative thoughts about oneself to evaluate participants’ overall sense of self-worth. The responses to each question are given on a 4-point Likert scale, with the options being ’strongly agree’ to ’strongly disagree.’ Higher ratings on the scale correspond to higher levels of self-esteem. It has been tested on samples of teenage girls from Nigeria 21. In this study, it was utilized to gauge the degree of adolescent self-esteem.
MINI-KID The Mini International Neuropsychiatric Interview version for children (MINI-KID) is a diagnostic interview specifically developed for children and adolescents aged 6–17 years 43. It was created to give clinicians a quick, valid, and accurate way to diagnose current DSM-IV and ICD-10 psychiatric illnesses and suicidality in child and adolescent populations. It generally has satisfactory psychometric properties, with excellent reliability estimates: kappa values of 1.00 and 0.72 for inter-rater and test-retest reliability 44. The MINI-KID was utilized to identify depressive disorders in the study sample. The MINI-KID’s current timeframe for the specific depressive disorders was adjusted for this investigation to the previous 12 months. It has been used in studies in Nigeria with good psychometric properties 45, 46.
Family APGAR The Family APGAR 47 is a brief screening questionnaire created to get a respondent’s opinion of how well their family is doing. It consists of five questions that measure how satisfied respondents are with each of the five aspects of family functioning: adaptability, partnership, growth, affection, and resolve. Each parameter is rated on a 3-point scale: 0 for rarely, 1 for occasionally, and 2 for almost always. A family with a total score of 0 to 3 is likely to be very dysfunctional, 4–6 is likely to be moderately dysfunctional, and 7 to 10 is likely to be highly functioning. In various local investigations, the Family APGAR Score is valid and accurate for evaluating family functioning 48,49. The participating students finished it without any assistance.
Data analysis
IBM SPSS statistics version 25.0 was used to analyze the study’s data. The independent t-test and analysis of variance (ANOVA) for continuous variables and chi-square statistics for categorical variables were used to evaluate the relationships between diagnostic categories and various sociodemographic, family, and psychosocial variables. Post-hoc analysis was conducted on statistically significant variables in the ANOVA analyses, and Fisher’s exact test was utilized as needed. Statistically significant variables in the bivariate analyses were entered into a multiple regression analysis model to identify independent predictors of depression. The Kolmogorov-Smirnov test was used to determine whether continuous variables such as age, FAPGAR score, overall academic exam score, and self-esteem score were normal.
Ethical approval
Ethical approval was obtained from the Ethical Committee of the Neuropsychiatric Hospital and the Ogun State Ministry of Education, Science, and Technology, and the administrators of the selected schools granted permission. The parents/guardians of all the participating students also provided written and signed informed consent forms. Additionally, it was made clear to the students that participation was voluntary. They could decide to withdraw from the study at any time, and not participating would not affect their academic performance. Teachers were not allowed in the room during the interviews to provide extra protection.
Results
A total of 225 students were selected to participate in the study, 5 (1.96%) of them declined to participate (they were all senior secondary school class 3 students; SSS 3 students) who had a significant test the next day, and 6 (2.35%) were excluded because they were older 18 years. The final sample size was 213.
Sociodemographic characteristics
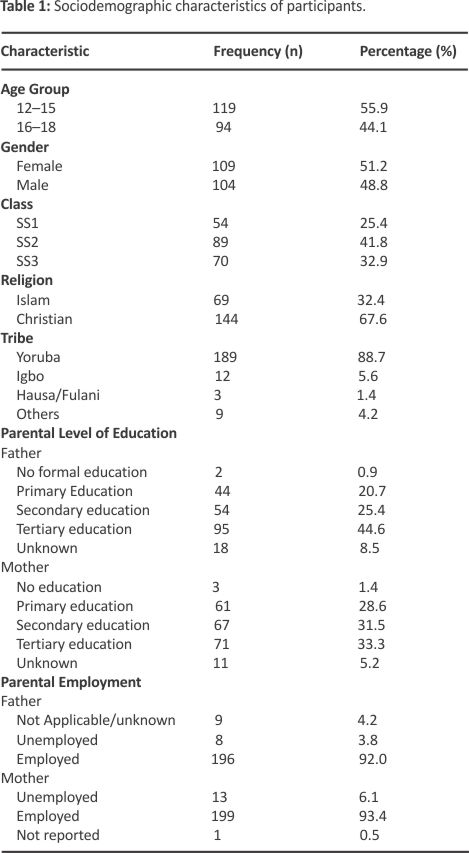
Table 1 summarizes the sociodemographic characteristics. The mean age was 15.3 years (SD = 1.27); 48.8% were male. Only 0.9% of fathers and 1.4% of mothers reported no formal education, and 3.8% of fathers were unemployed compared to 6.1%.
Child–related psychosocial factors
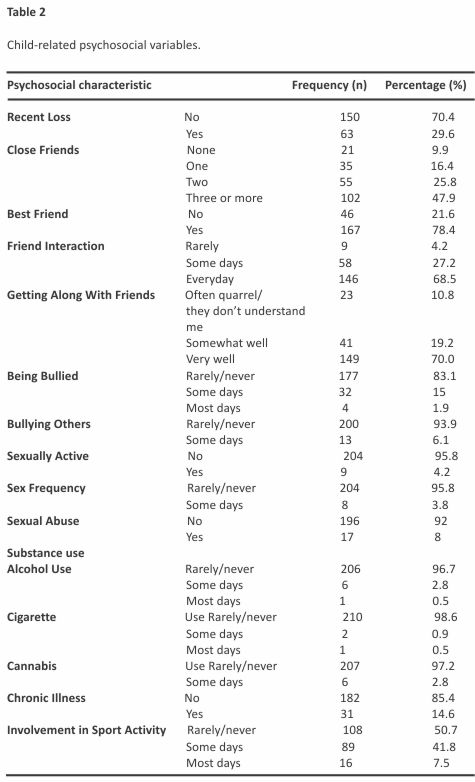
Table 2 shows child-related psycho-social factors. Sixty-three (29.6%) respondents experienced the loss of a close relative during the previous year; of these, 32 (50.8%) reported a close relationship with the deceased relative. Only 9.9% reported no friends; 13 (6.1%) people admitted to participating in bullying of others; 16.9% reported having experienced bullying; 17 (8.0%) participants had experienced sexual abuse (8.3% of girls vs 7.7% of boys); 16 (7.5%) people reported current use of psychoactive substances, with alcohol being the most popular drug (3.3%).
Academic performance
The respondents’ converted aggregate English and Mathematics scores ranged between 44 and 72. The median score was 56.0, while the mean score was 57.0 (SD = 6.4). There were no gender differences in academic performances, mean score for males was 57.42(SD = 6.8) compared to 56.61 (SD = 5.9) for females (t = -0.941; p = 0.348).
Rosenberg Self-Esteem Scale
The mean score for the whole sample was 19.07 (SD = 3.5). Boys reported higher scores compared to girls [19.55 (SD = 3.6) vs 18.61 (SD = 3.3; t = -1.997; p = 0.049].
Prevalence of depressive disorders
The twelve-month prevalence for any depressive disorder was 12.2%, major depressive disorder was 11.3% and dysthymia was 1.4%. Twelve-month prevalence for suicidality was 8.9%.
Correlates of depressive disorders
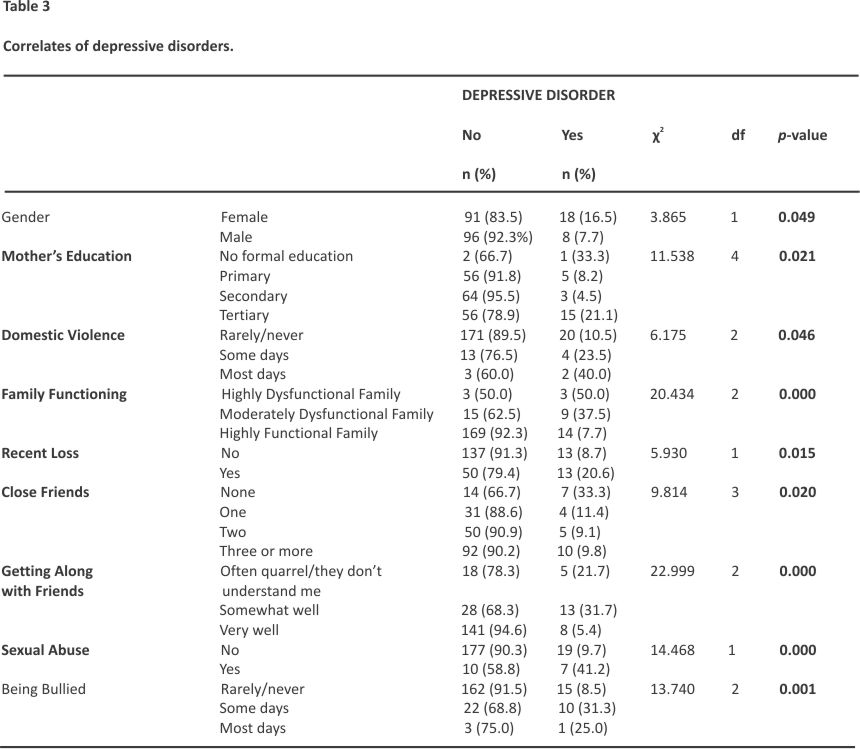
These are shown in Table 3. Female gender (p = 0.049); mother’s educational attainment (p = 0.021); perceived family dysfunction (p < 0.001); domestic violence (p = 0.046); history of sexual abuse (p < 0.001), being bullied (p = 0.001); experiencing a recent loss (p = 0.015); having fewer number of close friends (p = 0.020); and difficulty getting along with friends (p < 0.001) were all associated with depressive disorders. There was no association between age, parental psychopathology, sibship, single-parent household, polygamous family setting, use of psychoactive substances and chronic medical conditions, and depression.
Relationship between academic performance and disorder type
The aggregate English and mathematics exam scores were standardized to a normative mean of 50 and a standard deviation of 10. The standardization was done by obtaining a z score, which was multiplied by 10 and added to 50. The standardized scores were then compared between respondents diagnosed with depressive disorders vs. unaffected peers. Respondents with depressive disorder had a mean score of 44.71 (SD = 7.40), which was lower than the mean score of 50.74 (SD = 10.11) for non-depressed peers (t = 2.929; df = 211; p = 0.004).
Relationship between self-esteem and disorder type
Participants without depressive disorder had a mean score of 19.67 (SD = 3.181) compared to those with depressive disorder with a mean score of 16.42 (SD = 16.42), (F = 9.134, df = 3;209, p < 0.001).
Independent predictors of depressive disorders
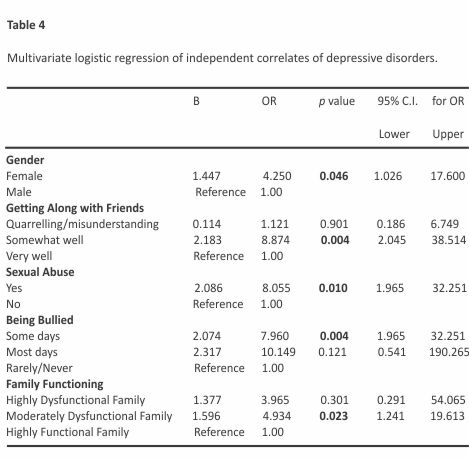
In the multivariate regression analyses (see Table 4), female gender (OR = 4.250; p = 0.046), moderate difficulty getting along with friends (OR = 7.502; p = 0.004), the experience of being occasionally bullied (OR = 7.960; p = 0.004), history of sexual abuse (OR = 8.055; p = 0.010) and moderate family dysfunction (OR = 4.934; p = 0.023) were associated with depression.
Discussion
This study aimed to determine the prevalence and correlates of depressive disorders among senior students attending secondary schools in Abeokuta. The twelve-month prevalence of any depressive disorder was 12.2%, and the major depressive episode was 11.3%.
Our study shows that depressive syndromes are a significant health burden in adolescents. The reported prevalence in this study is similar to that reported in other studies 1,2,22. The apparent convergence of rates is remarkable, given that these studies used different diagnostic instruments. Nevertheless, these findings are higher than elsewhere in Africa 7,36 and the West 50,51. Differing prevalence periods could explain the varied findings. In addition, the present study used a twelve-month window and found a rate closer to the lifetime rate reported in the US comorbidity survey 1; lower rates tended to be reported by studies using narrower time frames for prevalence rates.
The prevalence of dysthymia reported in this study was 1.4%, and to the best of the authors’ knowledge is the first estimate of the disorder among adolescents in Nigeria. The other available estimate on dysthymia comes from the Nigerian National Survey of Mental Health and Wellbeing (NSMHW) by Gureje et al., which found a twelve-month prevalence of 0.1% in the adult population 52. A similar prevalence rate of dysthymia has been reported in Norway 8 and Uganda 7. These findings may suggest that although depressive syndromes occur frequently among adolescents, only a small proportion of episodes tend to run prolonged episodes.
In the bivariate analysis, gender and mother’s education were the two sociodemographic variables significantly associated with depressive disorders in this study. This significant excess of females among adolescents having a depressive disorder has been replicated in many studies, both local and foreign 31,53. Gender difference in adolescence generally emerges in middle adolescence, typically by age 13,53. This has often led to suggestions that the female excess may be linked to pubertal changes in girls, specifically the achievement of Tanner stage III or IV 53. However, the changes in body morphology associated with puberty and their resultant psychosocial effects on social interactions and self-perception are insufficient to explain the female adolescent depression excess and underlying changes in androgen and estrogen levels may play a significant mediating role 54.
In this study, depressive disorders appeared to be more prevalent in adolescents with parents with lower educational attainment, although this difference was only significant for mothers’ educational attainment. Findings from elsewhere mostly report the reverse to be the case, i.e., adolescents with depression tend to have less educated parents 1,7,22. While it may be true that for some unknown reasons, depressive disorders occur more frequently in adolescents with better-educated parents in this population, the method of collating the information should be put in perspective. Adolescents’ self-reports on parental educational attainment might not be a reliable way of determining the parents’ highest level of education, so the findings should be interpreted with caution. Parental employment status, as reported by the adolescents, was the other approximate indicator of socio-economic status included in this study, the analysis of which showed that depression was more prevalent in respondents with unemployed parents. However, this difference was not found to be significant. Yet it appears more in keeping with the frequent associations observed between adolescent depression and low socioeconomic status in other studies 55.
The presence of a depressive disorder was significantly associated with the reported occurrence of domestic violence and perceived family dysfunction in this study, similar to findings elsewhere 7,22, 29,36. Persistent family disagreement through early adolescence increases the general level of low mood and depressive symptoms over time, and it is this rising level of non-clinical negative mood and thoughts that is associated with the onset of later clinical depression in older adolescents 30,56. Conversely, it may also be true that depressive symptoms in adolescents precipitate conflicts in an otherwise normally functioning family 24,57.
Reported traumatic experiences such as a recent loss within the last year, a history of sexual abuse, and being bullied were seen to be significantly associated with having a depressive disorder in this study, which is similar to other studies 29, 58. Classic Freudian theory which explains depression as aggression displaced from an external hostile object and turned inwards against the self, provides a psychodynamic framework for understanding this association. However, there is more evidence in the research base to support the cognitive formulation, which proposes that early adverse experiences could result in an enduring triad of negative cognitions about the self, the world, and the future, which then become embedded as a latent negative schema and is activated by subsequent events 59,60. The significant association between depression and the reported experience of being bullied may be explained by Seligman’s learned helplessness theory, which proposes that frequent exposure to uncontrollable and unpredictable events leads to an enduring loss of adaptive behaviours, eventually resulting in permanent deficits in cognitive and emotional processes 61.
Significant associations were also identified with impairments in peer relations in this study. Adolescents diagnosed with depressive disorder tended to report having fewer or no close friends at all and appeared to be experiencing difficulties getting along with friends. This agrees with findings by Field et al., who showed that depressed adolescents had less optimal peer relationships, fewer friends, and were less popular than unaffected peers 62. Although interpersonal difficulties appear more to be a consequence rather than an antecedent of depression in adolescents, there is evidence that heightened sociotropy (an increased need or desire for peer approval) in adolescents may render them more vulnerable to depression in the context of ongoing relational dysfunction with friends 62.
Regarding self-esteem, those with depressive disorders reported lower self-esteem compared to those who did not have depression, similar to other studies 21,22,63. Two possible models explain the observed strong link between depression and reduced self-esteem. The vulnerability model hypothesizes that low self-esteem is a risk factor for depression, whereas the scar model hypothesizes that low self-esteem is an outcome, not a cause, of depression. The direction of causality appears to have been resolved in favour of the vulnerability model by longitudinal studies utilizing cross-lagged regression analyses, which indicated that low self-esteem predicted subsequent levels of depression and not vice versa 63.
Depressive disorders were significantly associated with reduced academic performance in this study, which is similar to findings by Hysenbegasi and colleagues 64. Depression is associated with reduced volition, impaired concentration, and a general loss of interest in day-to-day tasks. Beyond potentially causing school absenteeism, affected adolescents might not fully engage in academic activities even when they attend school. Furthermore, intrinsic cognitive deficits are a recognized neuropsychological endophenotype of depression and may further limit academic performance even in the presence of sufficient engagement with school work 65.
In the multivariate regression analysis, female gender, the experience of bullying, difficulty getting along with friends, history of sexual abuse, lower self-esteem, and perceived family dysfunction were found to be independent predictors of depressive disorders, which is similar to what has been reported in other studies from around the world 1,21,22. Traumatic childhood experiences, in particular, are well-recognized as strong predictors for the subsequent onset of emotional disorders and even other psychiatric disorders 66, 67.
The regression model could only explain 50.2% of the variance in depressive illnesses in this study. This shows that a significant percentage of the variation in depressive disorders among adolescents may be explained by factors not considered in the current model, such as biological vulnerability. According to a meta-analysis of the genetic epidemiology of depression, the heritability was around 37% 68. Such additive genetic factors are thought to moderate the risk of the onset of major depression in part by altering the sensitivity of individuals to some of the depression-inducing psychosocial stressors identified in the present study.
This study comes with some limitations. Firstly, due to the study’s cross-sectional nature, causal inferences cannot be made. Secondly, the study was limited to a single city in the Southwest part of the country and may not be generalizable to adolescents in Nigeria. Thirdly, some of the questionnaires were self-reported and may be subject to response bias and social desirability bias, which may affect study validity. Fourth, the small sample size may limit the study’s power to detect statistically significant associations. Nevertheless, the final sample size was more than the calculated minimum sample size needed to detect a difference. The study also has strengths: this study went beyond the scope of previous work done in Nigeria on adolescent depression to investigate additional possible correlates, such as parental educational attainment. This study was also the first to report the prevalence of dysthymia among the adolescent population in Nigeria.
In conclusion, this study demonstrated that the prevalence of depressive illnesses in our environment is at par with reports from other parts of Africa and the rest of the world. The study also emphasized characteristics associated with depression, including being bullied, having a history of sexual abuse, having low self-esteem, and family dysfunctionality. Studies with larger adolescent samples that combine structured diagnostic interviews with self-report depression instruments in a two-stage design may be able to find other significant relationships that were missed in the current study. Our study’s findings underscore the importance of implementing depression screening initiatives for adolescents in secondary schools in Nigeria. Furthermore, we recommend providing training for guidance counsellors to effectively identify and address depression in students exhibiting declining academic performance. Additionally, the prevention of bullying is also an important strategy that should be implemented to curb the incidence of depression among adolescents in secondary schools in Nigeria.
Funding Statement
The author(s) received no specific funding for this work.
Data Availability
All relevant data are within the paper and its Supporting information files.
References
1. Merikangas KR, He J-p, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(10):980–9.
2. Abdulmalik JO, Omigbodun O, Wakil M, Beida O. Comorbidity of Depression with Substance Use among High School Students in Northern Nigeria. Addiction. 2012;5.
3. Osborn TL, Venturo-Conerly KE, Wasil AR, Schleider JL, Weisz JR. Depression and Anxiety Symptoms, Social Support, and Demographic Factors Among Kenyan High School Students. Journal of Child and Family Studies. 2020;29(5):1432–43.
4. Fatiregun A, Kumapayi T. Prevalence and correlates of depressive symptoms among in-school adolescents in a rural district in southwest Nigeria. Journal of Adolescence. 2014;37(2):197–203. doi: 10.1016/j.adolescence.2013.12. 003
5. Heron MP. Deaths: leading causes for 2017. National vital statistics reports. 2019.
6. Curtin SC, Warner M, Hedegaard H. Increase in suicide in the United States, 1999–2014: US Department of Health and Human Services, Centers for Disease Control and …; 2016.
7. Kinyanda E, Kizza R, Abbo C, Ndyanabangi S, Levin J. Prevalence and risk factors of depression in childhood and adolescence as seen in 4 districts of north-eastern Uganda. BMC international health and human rights. 2013;13:1–10.
8. Sund AM, Larsson B, Wichstrøm L. Prevalence and characteristics of depressive disorders in early adolescents in central Norway. Child and adolescent psychiatry and mental health. 2011; 5(1):1–13.
9. Kessler RC, Avenevoli S, R Merikangas K. Mood disorders in children and adolescents: an epidemiologic perspective. Biological psychiatry. 2001;49(12):1002–14. doi: 10.1016/ s0006-3223(01)01129-5
10. Lewinsohn PM, Rohde P, Seeley JR. Major depressive disorder in older adolescents: prevalence, risk factors, and clinical implications. Clinical psychology review. 1998;18(7):765– 94. doi: 10.1016/s0272-7358(98)000 10-5
11. Wilson S, Dumornay NM. Rising Rates of Adolescent Depression in the United States: Challenges and Opportunities in the 2020s. J Adolesc Health. 2022;70(3):354–5. doi: 10.1016/j.jadohealth.2021.12.003
12. Fleming JE, Offord DR. Epidemiology of childhood depressive disorders: A critical review. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29(4):571–80. doi: 10.1097/00004583-199007000-00010
13. Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of general psychiatry. 2003;60(8) :837– 44. doi: 10.1001/archpsyc. 60.8.837
14. Garber J. Depression in children and adolescents: linking risk research and prevention. American journal of preventive medicine. 2006;31(6): 104–25. doi: 10.1016/j.amepre. 2006.07.007
15. MacPhee AR, Andrews JJ. Risk factors for depression in early adolescence. Adolescence. 2006;41(163):435–66.
16. Wells VE, Deykin EY, Klerman GL. Risk factors for depression in adolescence. Psychiatric Developments. 1985;3(1) :83–108.
17. Greszta E. Family environment risk factors of depression in adolescence. Psychiatria Polska. 2006;40:719–30.
18. McGuffin P, Katz R, Watkins S, Rutherford J. A hospital-based twin register of the heritability of DSM-IV unipolar depression. Archives of general psychiatry. 1996;53(2):129–36. doi: 10.1001/archpsyc.1996.01830020047006
19. Strober M. Family-genetic aspects of juvenile affective disorders2001. 179–203 p.
20. Halligan SL, Murray L, Martins C, Cooper PJ. Maternal depression and psychiatric outcomes in adolescent offspring: a 13-year longitudinal study. Journal of Affective Disorders. 2007;97(1–3):145–54. doi: 10.1016/ j.jad.2006.06.010
21. Adewuya AO, Ologun YA. Factors associated with depressive symptoms in Nigerian adolescents. Journal of Adolescent Health. 2006;39(1):105 –10. doi: 10.1016/j.jadohealth.2005. 08.016
22. Lin HC, Tang TC, Yen JY, Ko CH, Huang CF, Liu SC, et al. Depression and its association with self-esteem, family, peer and school factors in a population of 9586 adolescents in southern Taiwan. Psychiatry and Clinical Neurosciences. 2008;62(4): 412–20. doi: 10.1111/j. 1440-1819. 2008.01820.x
23. Goodyer I, Herbert J, Tamplin A, Altham P. First-episode major depression in adolescents: Affective, cognitive and endocrine characteristics of risk status and predictors of onset. The British Journal of Psychiatry. 2000;176(2):142–9.
24. Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: the test of an interpersonal stress model in a community sample. Journal of consulting and clinical psychology. 2004;72(3):511. doi:10. 1037/0022-006X.72.3.511
25. Fendrich M, Warner V, Weissman MM. Family risk factors, parental depression, and psychopathology in offspring. Developmental psychology. 1990;26 (1):40.
26. Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Archives of general psychiatry. 2002;59(3):215–22. doi: 10.1001/archpsyc.59.3.215
27. Sagrestano LM, Paikoff RL, Holmbeck GN, Fendrich M. A longitudinal examination of familial risk factors for depression among inner-city African American adolescents. Journal of family psychology. 2003;17(1):108.
28. Lee J, Han C, Ko YH, Lee MS, Yoon HK. Assessment of life factors affecting the experience of depressive symptoms in adolescents: a secondary analysis using the Korea Youth Risk Behavior Survey. Child Adolesc Psychiatry Ment Health. 2021;15(1):50. doi: 10.1186/ s13034-021-00407-0
29. Zinzow HM, Ruggiero KJ, Resnick H, Hanson R, Smith D, Saunders B, et al. Prevalence and mental health correlates of witnessed parental and community violence in a national sample of adolescents. Journal of Child Psychology and Psychiatry. 2009;50(4):441–50. doi: 10.1111/j. 1469-7610.2008.02004.x
30. Sternberg KJ, Lamb ME, Guterman E, Abbott CB. Effects of early and later family violence on children’s behaviour problems and depression: A longitudinal, multi-informant perspective. Child abuse & neglect. 2006;30(3):283 –306. doi: 10.1016/j.chiabu.2005. 10.008
31. Adeniyi AF, Okafor NC, Adeniyi CY. Depression and physical activity in a sample of Nigerian adolescents: levels, relationships and predictors. Child and adolescent psychiatry and mental health. 2011;5:1–10.
32. Cairns RB, Leung MC, Buchanan L, Cairns BD. Friendships and social networks in childhood and adolescence: Fluidity, reliability, and interrelations. Child development. 1995;66(5):1330–45.
33. Reinherz HZ, Giaconia RM, Pakiz B, Silverman AB, Frost AK, Lefkowitz ES. Psychosocial risks for major depression in late adolescence: A longitudinal community study. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(6):1155–63. doi: 10.1097/00004583-199311000-00007
34. Kaltiala-Heino R, Rimpelä M, Marttunen M, Rimpelä A, Rantanen P. Bullying, depression, and suicidal ideation in Finnish adolescents: school survey. Bmj. 1999;319(7206):348–51. doi: 10.1136/bmj.319.7206.348
35. B Klomek A, Marrocco F, Kleinman M, Schonfeld IS, Gould MS. Bullying, depression, and suicidality in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2007; 46(1):40–9. doi: 10.1097/01.chi.000 0242237.84925.18
36. Adewuya AO, Ola BA, Aloba OO. Prevalence of major depressive disorders and a validation of the Beck Depression Inventory among Nigerian adolescents. European Child & Adolescent Psychiatry. 2007;16: 287–92. doi: 10.1007/s00787-006-0557-0
37. Abbo C, Kinyanda E, Kizza RB, Levin J, Ndyanabangi S, Stein DJ. Prevalence, comorbidity and predictors of anxiety disorders in children and adolescents in rural north-eastern Uganda. Child and adolescent psychiatry and mental health. 2013;7(1):1–11.
38. Muris P, Schmidt H, Engelbrecht P, Perold M. DSM-IV–defined anxiety disorder symptoms in South African children. Journal of the American Academy of Child & Adolescent Psychiatry. 2002; 41(11):1360–8. doi: 10.1097/0000 4583-200211000-00018
39. Ndetei DM, Khasakhala L, Nyabola L, Ongecha-Owuor F, Seedat S, Mutiso V, et al. The prevalence of anxiety and depression symptoms and syndromes in Kenyan children and adolescents. Journal of Child & Adolescent Mental Health. 2008;20(1):33–51. doi: 10.2989/JCAMH.2008.20.1.6.491
40. Nzeakah C W, DadeMatthews AO, Onofa U O, DadeMatthews O D, O T. Crippled By Fear: Anxiety Disorders Among Adolescents In Nigeria. International Journal of Psychiatry. 2022;7(2):103–15.
41. Araoye MO. Research methodology with statistics for health and social sciences. Ilorin: Nathadex Publisher; 2003. 25–120 p.
42. Rosenberg M. Society and the adolescent self-image.(revised edition). Middletown, Connecticut Wesleyan University Press; 1989.
43. Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(20):22–33.
44. Sheehan DV, Sheehan KH, Shytle RD, Janavs J, Bannon Y, Rogers JE, et al. Reliability and validity of the mini international neuropsychiatric interview for children and adolescents (MINI-KID). The Journal of Clinical Psychiatry. 2010;71(3):17393. doi: 10.4088/JCP. 09m05305whi
45. Adegunloye O, Yusuf A, Ajiboye P, Issa B, Buhari O. Prevalence and Correlates of Distruptive Behaviour Disorders in Youths in a Juvenile Borstal Institution. Niger J Psychiatry. 2010;8(3):12–7.
46. Adeyemo S, Adeosun II, Ogun OC, Adewuya A, David AN, Adegbohun AA, et al. Depression and suicidality among adolescents living with human immunodeficiency virus in Lagos, Nigeria. Child and Adolescent Psychiatry and Mental Health. 2020;14:1–10.
47. Smilkstein G. The family APGAR: a proposal for a family function test and its use by physicians. J fam pract. 1978;6(6):1231–9.
48. Eseigbe E, Eseigbe P, Nuhu F, Sheikh T, Majebi M, Kalu A, et al. Impact of childhood mental health disorders on the family: A Case report. Nigerian Journal of Paediatrics. 2013;40(4): 419–21.
49. Muyibi AS, Ajayi I-OO, Irabor AE, Ladipo MM. Relationship between adolescents’ family function with sociodemographic characteristics and behaviour risk factors in a primary care facility. African Journal of Primary Health Care and Family Medicine. 2010;2(1):1–7.
50. Jane Costello E, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? Journal of child psychology and psychiatry. 2006;47(12):1263–71. doi: 10.1111/ j.1469-7610.2006.01682.x
51. Maughan B, Collishaw S, Stringaris A. Depression in childhood and adolescence. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2013;22(1):35.
52. Gureje O, Lasebikan VO, Kola L, Makanjuola VA. Lifetime and 12-month prevalence of mental disorders in the Nigerian Survey of Mental Health and Well-Being. The British Journal of Psychiatry. 2006;188(5): 465–71. doi: 10.1192/bjp.188.5.465
53. Angold A, Costello EJ. The epidemiology of depression in children and adolescents. The depressed child and adolescent, 2nd ed. Cambridge child and adolescent psychiatry. New York, NY, US: Cambridge University Press; 2001. p. 143–78.
54. Angold A, Costello E, Erkanli A, Worthman C. Pubertal changes in hormone levels and depression in girls. Psychological medicine. 1999; 29(5):1043–53. doi: 10.1017/s0033 291799008946
55. Xu F, Cui W, Xing T, Parkinson M. Family Socioeconomic Status and Adolescent Depressive Symptoms in a Chinese Low- and middle-income Sample: The Indirect Effects of Maternal Care and Adolescent Sense of Coherence. Front Psychol. 2019;10:819. doi: 10.3389/fpsyg.2019.00819
56. Rueter MA, Scaramella L, Wallace LE, Conger RD. The first onset of depressive or anxiety disorders is predicted by the longitudinal course of internalizing symptoms and parent-adolescent disagreements. Archives of general psychiatry. 1999;56(8):726–32. doi: 10. 1001/archpsyc.56.8.726
57. Hammen C, Rudolph K, Weisz J, Rao U, Burge D. The context of depression in clinic-referred youth: Neglected areas in treatment. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(1): 64–71. doi: 10.1097/00004583-199901000-00021
58. Nguyen DT, Dedding C, Pham TT, Wright P, Bunders J. Depression, anxiety, and suicidal ideation among Vietnamese secondary school students and proposed solutions: a cross-sectional study. BMC Public Health. 2013;13:1– 10.
59. Beck AT. Cognitive therapy of depression: Guilford Press; 1979.
60. Lewinsohn PM, Clarke GN. Psychosocial treatments for adolescent depression. Clinical psychology review. 1999; 19(3):329–42. doi: 10.1016/s0272-7358(98)00055-5
61. Seligman ME. On depression, development, and death1975.
62. Field T, Diego M, Sanders C. Adolescent depression and risk factors. Adolescence. 2001;36(143):491–8.
63. Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. 2013;139(1):213–40. doi: 10.1037/a0028931
64. Hysenbegasi A, Hass SL, Rowland CR. The impact of depression on the academic productivity of university students. Journal of mental health policy and economics. 2005;8(3):145.
65. Bulbena A, Berrios G. Cognitive function in the affective disorders: a prospective study. Psychopathology. 1993;26(1):6–12. doi: 10.1159/0002 84794
66. Bender K, Brown SM, Thompson SJ, Ferguson KM, Langenderfer L. Multiple victimizations before and after leaving home associated with PTSD, depression, and substance use disorder among homeless youth. Child maltreatment. 2015;20(2): 115–24. doi: 10.1177/10775595145 62859
67. Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological medicine. 1997; 27(5):1101–19. doi: 10.1017/s00332 91797005588
68. Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. American journal of psychiatry. 2000; 157(10):1552–62. doi: 10.1176/appi. ajp.157.10.1552
CREDITS: DadeMatthews A, Nzeakah C, Onofa L, DadeMatthews O, Ogundare T. Teenage Blues: Predictors of depression among adolescents in Nigeria. PLoS One. 2024 Apr 17;19(4):e0293995. doi: 10.1371/journal.pone.0293995. PMID: 38630744; PMCID: PMC11023510.











