Emma J. Derbyshire1 * and Philip C. Calder2,3
1Nutritional Insight, London, United Kingdom
2Faculty of Medicine, School of Human Development and Health, University of Southampton, Southampton, United Kingdom
3National Institute for Health Research Southampton Biomedical Research Center, University Hospital Southampton National Health Service Foundation Trust and University of Southampton,
Southampton, United Kingdom
*Correspondence: Emma J. Derbyshire, emma@nutritional-insight.co.u
Upper and lower respiratory tract infections are among the most common infections globally, and in the United Kingdom, they account for about half of all oral antibiotics prescribed. Antibiotic overuse and the emergence of “superbugs” that are resistant to their effects is a global problem that is becoming a serious concern. Considering this, the potential role of immunonutrition as a “prehabilitation” in helping to tackle bacterial infections and reduce over-reliance on antibiotic usage is gaining interest. This narrative mini-review summarizes current knowledge on the roles of certain nutrients in helping to modulate immune function, with particular focus on vitamin D. Vitamin D supplementation appears to reduce the risk of acute respiratory tract infections and thus could have a valuable role to play in reducing over-reliance on antibiotics. Investment in high-quality trials is needed to further explore this field.
Keywords:
respiratory tract infections, antibiotic resistance, vitamin D, immunonutrition, prehabilitation
Introduction
There has been an upsurge of novel bacterial, viral, and fungal respiratory pathogens that are becoming increasingly challenging to treat, with respiratory tract infections (RTIs) being exacerbated by antibiotic resistance of Gram-positive and Grain-negative bacteria 1. Acute respiratory tract infections (ARTIs), which include upper respiratory tract infections (URTIs), are, among adults, the most common cause of antibiotic prescription 2. In the United Kingdom, an examination of over eight million patient records from 587 general practices showed that URTIs accounted for around 31% of oral antibiotic prescriptions and lower respiratory tract infections (LRTIs) accounted for around 19% 3.
The very first antibiotic, salvarsan, was developed in 1910 while penicillin discovery by Alexander Fleming followed in 1928 4. Multiple antibiotics have been discovered since then, but now, after about 100 years of the “antibiotic era,” fewer new antibiotics are being identified and significant antibiotic resistance has emerged 4. The World Health Organization considers that the unprecedented use of antibiotics and subsequent antimicrobial resistance (AMR) is currently one of the largest threats to global health, food security, and human development 5, 6.
In 2016, ARTIs were responsible for ~2.38 million deaths globally 7,8. Within the European Union, 25,000 people have been estimated to die annually because of AMR with resultant societal costs of around 1.5 billion euros annually 9. By 2050, it has been estimated that some 10 million people globally could die annually as a result of AMR—with 390,000 Europeans estimated to be affected and even larger proportions of Asian (4,730,000) and African (4,140,000) populations 6. It has been further predicted that standard antibiotic treatments may no longer work, subsequently making infections more difficult to treat and control 10.
Given the high prevalence of ARTIs coupled with rising rates of AMR, novel approaches are needed for the future. The concept of “prehabilitation,” including the role of immunonutrition, could play a pivotal role in helping to both prevent and offset RTIs should these occur. Prehabilitation has been well defined elsewhere as: “interventions that can help to improve patient’s health in advance of being exposed to a physiological stressor so they are then better able to cope with that stress” 11. This narrative mini-review describes how immunonutrition could become a valuable tool in conventional medicine. It focuses on ARTIs and vitamin D, for which there is an expanding body of evidence.
Nutrition, Infection, and Immunity
The roles of nutrients in supporting the function of the immune system are numerous and varied, with an adequate and balanced supply of nutrients being required if a suitable immune response is to be mounted 12. The immune system protects the body against infectious agents and is composed of innate responses—the body’s first lines of defence—and adaptive responses that generate immunological memory 13. It is known that a bidirectional relationship exists between nutrition, infection, and immunity with changes in one impacting on each of the others 14. Micronutrients (vitamins and minerals) have extended roles influencing and supporting every stage of the human immune response 13. Subsequently, deficiencies in one or more micronutrients can affect both innate and adaptive immunity, resulting in immunosuppression and exacerbating susceptibility to infections 13.
A host of nutrients have been implicated as being essential for immunocompetence, including vitamins A, B2, B6, B9 (folic acid), B12, C, D, E, and iron, zinc, selenium, copper, and magnesium 14. Vitamins A, C, D, E, and zinc are important for the structural and functional integrity of the body’s external and mucosal barriers to invading pathogens 15. Cellular processes of both innate and adaptive immunity, such as cell differentiation and proliferation, phagocytosis, respiratory burst, killing activity, cytokine production, and antibody production are all dependent on suitable amounts of vitamins A, D, C, E, B6, and B12, folate, iron, zinc, copper, selenium, and magnesium15.
This mini-review focuses on vitamin D, due to the growing body of evidence favouring a role for vitamin D in preventing ARTIs. Vitamin D augments host barrier epithelial integrity by reinforcing intercellular junctions 16. It has also been found to trigger antimicrobial peptide production, which exhibits direct pathogen-killing capacity 17. The vitamin D receptor is expressed on many immune cell types including B-cells, T-cells, and antigen-presenting cells 18–20. Furthermore, some immune cell types, including macrophages and dendritic cells, can synthesize the active form of vitamin D, 1,25-dihydroxyvitamin D3 21. These two observations suggest high importance for vitamin D within the immune system. Indeed, vitamin D deficiency results in impaired localized innate immunity and a defective antigen-specific cellular immune response, correlated with a higher susceptibility to infections 22. Vitamin D metabolites have also been found to influence the expression and secretion of pro-inflammatory chemokines and cytokines 23, and vitamin D promotes the production of anti-microbial peptides such as cathelicidin 21, 24.
An established body of evidence now shows that 1,25-dihydroxyvitamin D3 influences endothelial membrane stability and acts on multiple parts of the innate and adaptive immune responses 21. Low levels of 1,25-dihydroxyvitamin D3 correlate with an increased risk of developing several immune-related disorders including respiratory infection and COVID-19 21. Vitamin D has further been found to be involved in pulmonary angiotensin-converting enzyme 2 expressions and has the ability to reduce lung surface tension in COVID-19 25. Other work suggests that vitamin D may induce progesterone-induced blocking factor and exert inhibitory effects on inflammation including the cytokine IL-6, which tend to be elevated in COVID-19 26.
Vitamin D and RTIs
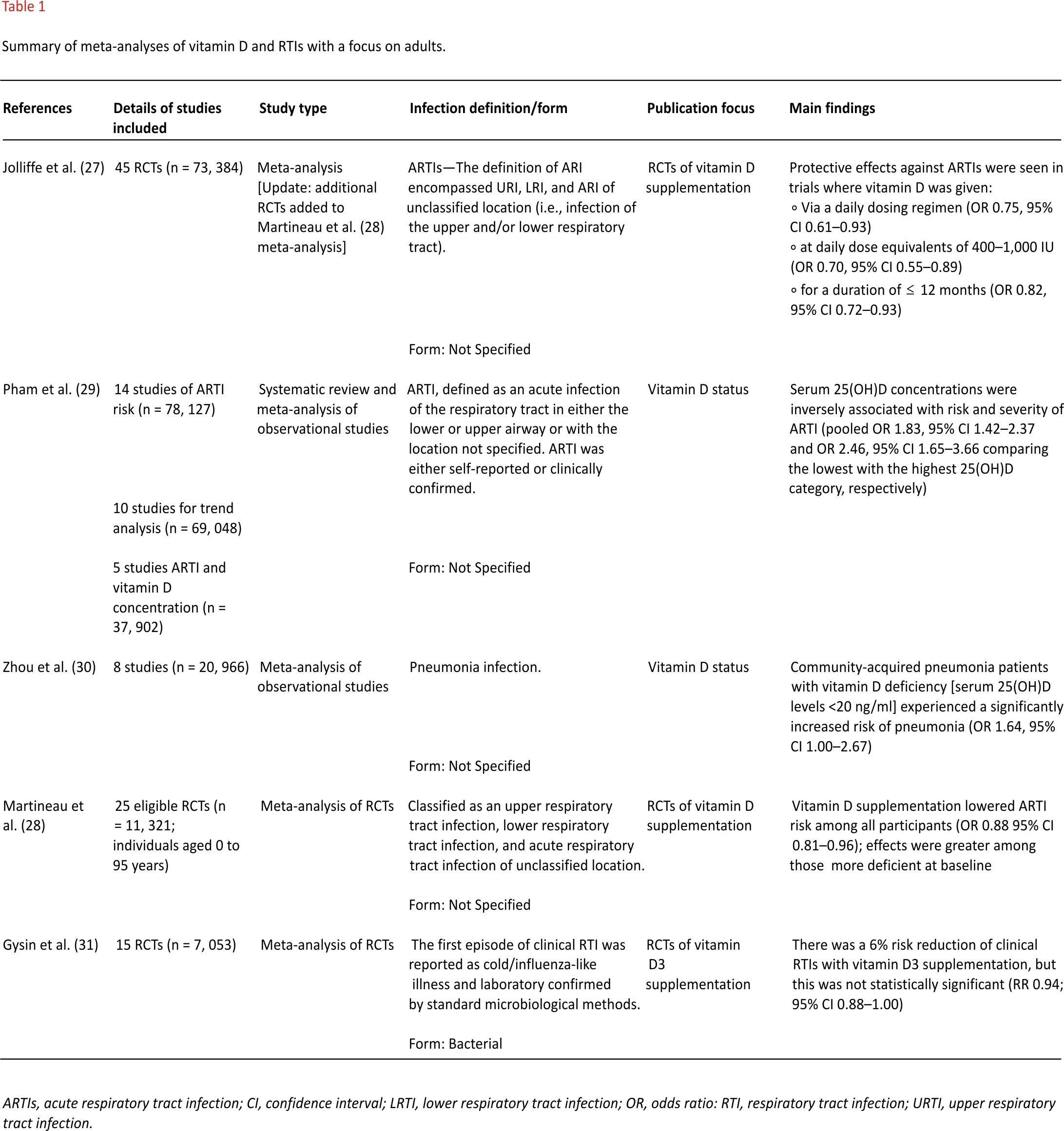
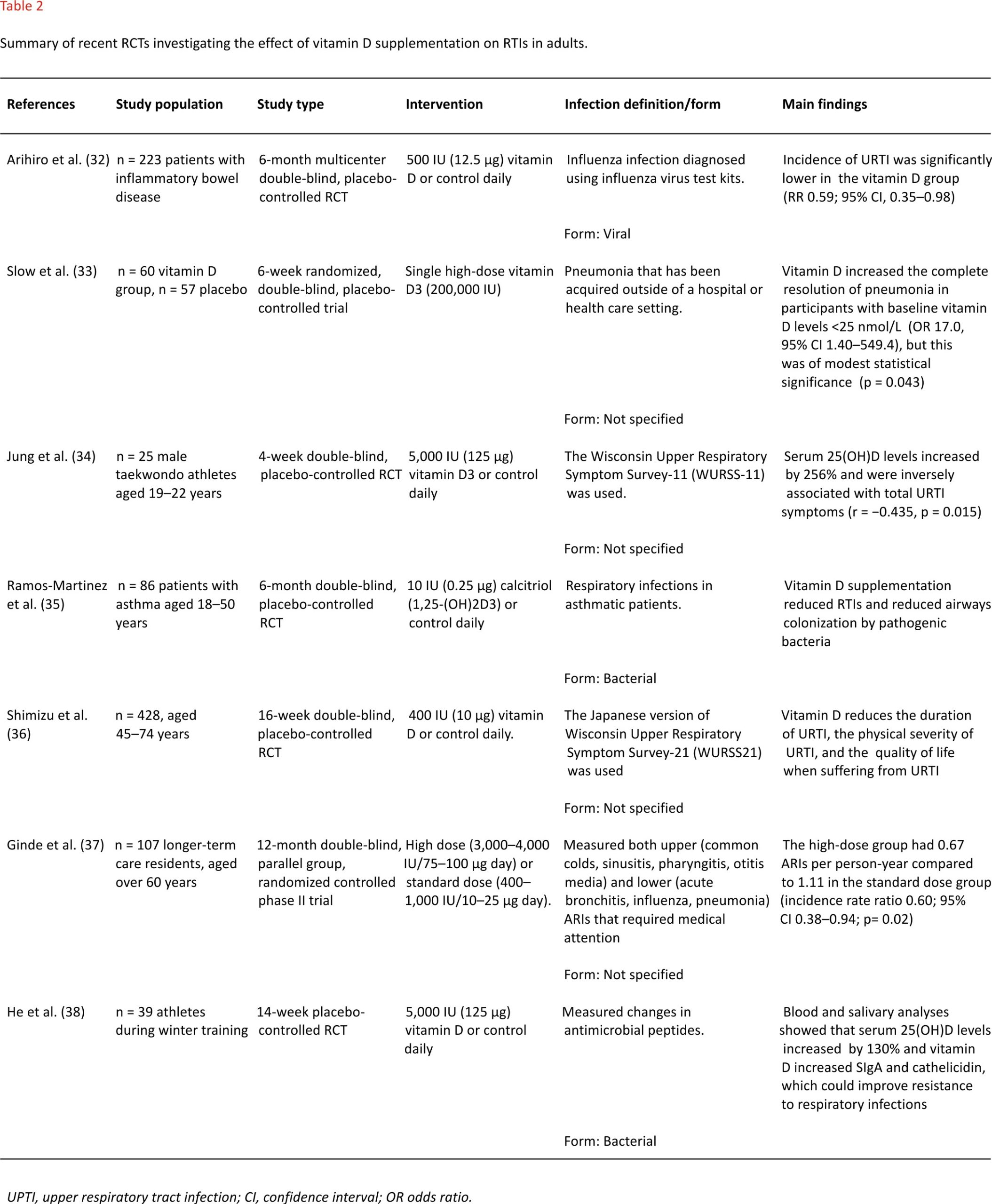
A growing number of studies have investigated the role of vitamin D on the occurrence of ARTIs. Table 1 summarizes evidence from meta-analyses and Table 2 summarizes evidence from RCTs, published in the last 5 years with a focus on adulthood, although some meta-analyses included extended age ranges.
Two meta-analyses focused on observational research 29,30 and four focused on evidence from RCTs 27,28,31. Those collating observational findings found inverse relationships between serum 25-hydroxyvitamin D levels and risk and severity of ARTIs 29 and risk of community-acquired pneumonia 30. Meta-analyses pooling evidence from RCTs focused on findings from vitamin D supplementation programs represent a higher level of evidence since they can establish a cause-and-effect relationship. The largest meta-analysis included data from 45 RCTs (n = 73,384 subjects) concluding that daily dosing regimens providing 400–1,000 IU (10–25 μg) of vitamin D were most effective at protecting against ARTIs 27. Earlier meta-analyses reported similar findings: that vitamin D supplementation lowered ARTI risk 28, particularly among those with profound 25-hydroxyvitamin D deficiency at baseline 28. Focusing on vitamin D supplementation, a separate meta-analysis (15 RCTs, n = 7053) observed a 6% risk reduction of clinical RTIs, but this was not statistically significant and heterogeneity among the included studies was high (I2= 57%) 31.
Evidence from individual RCTs has reported similar findings. Five studies reported that vitamin D supplementation reduced the incidence 32,35,37, duration and severity 36, and symptoms 34 of RTIs. Among asthmatic patients, Ramos-Martinez et al. observed that vitamin D reduced RTIs, an effect that correlated with higher sputum levels of IL-10, IFN-γ, and cathelicidin LL-37 35. Vitamin D dosages used among the different studies were highly variable, ranging from just 10 IU (0.25 μg daily) 35 up to 4,000 IU (100 μg daily) 37. Similarly, the duration of RCTs was also wide-ranging, with the shortest being 4 weeks 34 and the longest, conducted in health care residents, being over a 12-month period 37.
Regarding the pathological cause of infection, only four studies clearly specified whether these were bacterial 31,35,38 or viral 32. The remaining studies focused on the location, duration, and/ or severity of RTIs, but their source was not clearly defined or diagnosed.
Discussion and Conclusions
Presently, vitamin D guidelines in the United Kingdom have been set at 10 μg daily from October to March to keep bones, teeth, and muscles healthy 39. However, given updated meta-analytical evidence and a growing number of RCTs, combined with the global COVID-19 pandemic, it seems timely that this advice should be updated to encompass respiratory health with the required supplemental dose being re-evaluated. Clearly, vitamin D intakes should conform to recommended upper safety limits established by expert authorities with the European Food Safety Authority setting an upper limit of 100 μg/day for adults, including pregnant and lactating women 40. Equally, supplementation should always be in addition to the consumption of a healthy, varied, and well-balanced diet. Nevertheless, a more desirable level of intake of vitamin D taking the latest evidence into account would be 2,000 IU (50 μg) daily to reduce the risk of ARTIs 41.
Regarding antibiotic use, more clinical studies evaluating the impact of vitamin D are needed as an outcome alongside ARTI incidence, symptoms, and severity. One Cochrane review evaluated evidence from seven studies where vitamin D was used as an adjunct to antibiotics to treat pneumonia, but findings were inconclusive 42. In Sweden, vitamin D3 supplementation [1,500–1, 600 IU (37.5–40 μg) daily over 12 months] was found to significantly reduce antibiotic usage—from 20 to 15 days per person 43. Equally, future studies should clearly define the origin of pathological RTIs. It is possible that different vitamin D dosing regimens may be warranted for viral and bacterial infections, but there is presently not enough evidence to draw firm conclusions on this.
AMR poses a threat to future global health, and the current COVID-19 pandemic is highly damaging to health, societies, and economies. Urgent responses are needed. Supporting the immune system of the population in advance of exposure to infections (i.e., “immune prehabilitation”) would reduce the number and severity of infections and reduce the use of antibiotics. Vitamin D has multiple roles in supporting the immune system 21,44,45 and evidence from RCTs demonstrates that supplemental vitamin D reduces the risk of acquiring RTIs 32,35,37 as well as their duration and severity 34,36 and may reduce antibiotic use 43. There is also evidence that individuals with better vitamin D status are less likely to develop COVID-19 and severe COVID-19 46–48. Given these observations, the guidance of vitamin D intake should consider immune health, in addition to bone, tooth, and muscle health. Higher vitamin D intake in the population would reduce infections, result in infections being less severe and reduce the use of antibiotics. The RCTs that form the current evidence base have highly variable designs including substantial differences in dose of vitamin D used, regularity of dosing, and duration of dosing. Thus, further clinical trials and meta-analytical approaches are warranted to clarify matters of dose, dosing regimen, and the precise relationship between vitamin D status and immune and respiratory health in different groups of the population including older people and different ethnicities.
Author Contributions
ED and PC compiled, researched, wrote, and edited the review.
Conflict of Interest
ED is the founder of Nutritional Insight.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Zumla A, Memish ZA, Maeurer M, Bates M, Mwaba P, Al-Tawfiq JA, et al. Emerging novel and antimicrobial-resistant respiratory tract infections: new drug development and therapeutic options. Lancet Infect Dis. (2014) 14:1136–49. doi: 10.1016/ S1473-3099 (14)70828-X
2. Harris A, Hicks L, Qaseem A. Appropriate antibiotic use for acute respiratory tract infection in adults: advice for high-value care from the American College of Physicians and the Centers for Disease Control and Prevention. High-Value Care Task Force of the American College of Physicians and for the Centers for Disease Control and Prevention. Ann Intern Med. (2016) 164:425–34. doi: 10.7326/ M15-1840
3. Palin V, Molter A, Belmonte M, Ashcroft DM, White A, Welfare W, et al. Antibiotic prescribing for common infections in UK general practice: variability and drivers. J Antimicrob Chemother. (2019) 74: 2440–50. doi: 10.1093/jac/dkz163
4. Hutchings MI, Truman AW, Wilkinson B. Antibiotics: past, present and future. Curr Opin Microbiol. (2019) 51:72–80. doi: 10.1016/j.mib. 2019. 10.008
5. WHO. Antibiotic Resistance. (2020). Available online at: https://www. who. int/news-room/fact-sheets/detail/ antibiotic-resistance
6. O’Neill J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. (2014). Available online at: https://amr-review.org/ sites/default/files/AMR%20Review%20 Paper%20-%20Tackling%20a% 20crisis%20for%20the%20health %20and%20wealth%20of%20nations_1.pdf
7. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016 GBD 2016. Causes of Death Collaborators. Lancet. (2017) 390: 1151–210. doi: 10.1016/S01 40-6736 (17)32152-9
8. GBD 2016b Lower Respiratory Infections Collaborators. Estimates of the global, regional, national morbidity. mortality, and aetiologies of lower respiratory infections in 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. (2018) 18:1191– 210. doi: 10.1016/S1473-3099(18) 30310-4
9. HPRA. Health Products Regulatory Authority. Report on Antimicrobial Resistance, Dublin (2016).
10. WHO. Antimicrobial Resistance. Global Report on Surveillance, Switzerland (2014).
11. Silver J. Prehabilitation could save lives in a pandemic. BMJ. (2020) 369:m 1386. doi: 10.1136/bmj.m 1386
12. Calder P. Nutrition, immunity and COVID-19. BMJ Nutr Prev Health. (2020) 3:74–92. doi: 10.1136/bmj nph-2020-000085
13. Pecora F, Persico F, Argentiero A, Neglia C, Esposito S. The role of micronutrients in support of the immune response against viral infections. Nutrients. (2020) 12:31 98. doi: 10.3390/nu1 2103198
14. Maggini S, Pierre A, Calder PC. Immune function and micronutrient requirements change over the life course. Nutrients. (2018) 10:1531. doi: 10.3390/nu101 01531
15. Gombart AF, Pierre A, Maggini S. A review of micronutrients and the immune system-working in harmony to reduce the risk of infection. Nutrients. (2020) 12:236. doi: 10.3390/nu1 2010 236
16. Fakhoury HMA, Kvietys PR, AlKattan W, Anouti FA, Elahi MA, Karras SN, et al. Vitamin D and intestinal homeostasis: barrier, microbiota, immune modulation. J Steroid Biochem Mol Biol. (2020) 200:105663. doi:10.1016/j.jsbmb. 2020.105663
17. Korf H, Decallonne B, Mathieu C. Vitamin D for infections. Curr Opin Endocrinol Diabetes Obes. (2014) 21:431–6. doi: 10.1097/ MED.0000 000000000108
18. Aranow C. Vitamin D and the immune system. J Investig Med. (2011) 59: 881 –6. doi: 10.2310/JIM.0b013e3 1821b8755
19. Borges MC, Martini LA, Rogero MM. Current perspectives on vitamin D, immune system, chronic diseases. Nutrition. (2011) 27:399–404. doi: 10.1016/j.nut.2010.07.022
20. Mora JR, Iwata M, Andrian von UH. Vitamin effects on the immune system: vitamins A and D take centre stage. Nat Rev Immunol. (2008) 8:685–98. doi: 10.1038/nri2378
21. Charoenngam N, Holick MF. Immunologic effects of vitamin D on human health and disease. Nutrients. (2020) 12:20 97. doi: 10.3390/nu12072097
22. Wintergerst ES, Maggini S, Hornig DH. Contribution of selected vitamins and trace elements to immune function. Ann Nutr Metab. (2007) 51:301–23. doi: 10.1159/0001076 73
23. Greiller CL, Martineau AR. Modulation of the immune response to respiratory viruses by vitamin D. Nutrients. (2015) 7:4240–70. doi: 10.3390/nu7064240
24. Chung C, Silwal P, Kim I, Modlin RL, Jo EK. Vitamin D-Cathelicidin Axis: at the Crossroads between Protective Immunity and Pathological Inflammation during Infection. Immune Netw. (2020)20: e12.doi: 10.4110/in.2020.20.e12
25. Ebadi M, Montano-Loza AJ. Perspective: improving vitamin D status in the management of COVID-19. Eur J Clin Nutr. (2020) 74:856–9. doi: 10.1038 /s41430-020-0661-0
26. Orru B, Szekeres-Bartho J, Bizzarri M, Spiga AM, Unfer V. Inhibitory effects of Vitamin D on inflammation and IL-6 release. Further support for COVID-19 management? Eur Rev Med Pharmacol Sci. (2020) 24:8187–93. doi: 10.26355 /eurrev _202008_22507
27. Jolliffe DA, Camargo CA, Sluyter JD, Aglipay M, Aloia JF, Ganmaa D, et al. Vitamin D supplementation to prevent acute respiratory infections: systematic review and meta-analysis of aggregate data from randomised controlled trials. medRxiv [Preprint]. (2020). doi:10. 1101/2020.07.14.20152728
28. Martineau AR, Jolliffe DA, Greenberg L, Aloia JF, Bergman P, Dubnov-Raz G, et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol Assess. (2019) 23:1–44. doi: 10.3310/hta230 20
29. Pham H, Rahman A, Majidi A, Waterhouse M, Neale RE. Acute respiratory tract infection and 25-hydroxyvitamin d concentration: a systematic review and meta-analysis. Int J Environ Res Public Health. (2019) 16:3020. doi: 10. 3390/ijerph16173020
30. Zhou YF, Luo BA, Qin LL. The association between vitamin D deficiency and community-acquired pneumonia: a meta-analysis of observational studies. Medicine (Baltimore). (2019) 98:e1 7252. doi: 10.1097/MD.00000000000 1 7252
31. Gysin DV, Dao D, Gysin CM, Lytvyn L, Loeb M. Effect of Vitamin D3 Supplementation on respiratory tract infections in healthy individuals: a systematic review and meta-analysis of randomized controlled trials. PLoS One. (2016) 11:e0162996. doi: 10.1371 /journal.pone.016 2996
32. Arihiro S, Nakashima A, Matsuoka M, Suto S, Uchiyama K, Kato T, et al. Randomized trial of vitamin D supplementation to prevent seasonal influenza and upper respiratory infection in patients with inflammatory bowel disease. Inflamm Bowel Dis. (2019) 25:1088–95. doi: 10.1093/ ibd/izy346
33. Slow S, Epton M, Storer M, Thiessen R, Lim S, Wong J, et al. Effect of adjunctive single high-dose vitamin D3 on the outcome of community-acquired pneumonia in hospitalised adults: the VIDCAPS randomised controlled trial. Sci Rep. (2018) 8:13829. doi: 10.1038/ s41598-018-32162-2
34. Jung HC, Seo MW, Lee S, Kim SW, Song JK. Vitamin D(3) Supplementation reduces the symptoms of upper respiratory tract infection during winter training in vitamin D-insufficient taekwondo athletes: a randomized controlled trial. Int J Environ Res Public Health. (2018) 15:2003. doi: 10.3390 /ijerph150920 03
35. Ramos-Martinez E, Lopez-Vancell MR, Fernandez de Cordova-Aguirre JC, Rojas-Serrano J, Chavarria A, Velasco-Medina A, et al. Reduction of respiratory infections in asthma patients supplemented with vitamin D is related to increased serum IL-10 and IFNgamma levels and cathelicidin expression. Cytokine. (2018) 108: 239–46. doi: 10.1016/ j.cyto.2018.01. 001
36. Shimizu Y, Ito Y, Yui K, Egawa K, Orimo H. Intake of 25-hydroxyvitamin D3 reduces duration and severity of upper respiratory tract infection: a randomized, double-blind, placebo-controlled, parallel-group comparison study. J Nutr Health Aging. (2018) 22:491–500. doi: 10.1007/s12603-017-0952-x
37. Ginde AA, Blatchford P, Breese K, Zarrabi L, Linnebur SA, Wallace JI, et al. High-Dose Monthly vitamin D for prevention of acute respiratory infection in older long-term care residents: a randomized clinical trial. J Am Geriatr Soc. (2017) 65:496–503. doi: 10.1111/jgs.14679
38. He CS, Fraser WD, Tang J, Brown K, Renwick S, Rudland-Thomas J, et al. The effect of 14 weeks of vitamin D3 supplementation on antimicrobial peptides and proteins in athletes. J Sports Sci. (2016) 34:67–74. doi: 10.1080/02640 414.2015.1033642
39. NICE NICE PHE and SACN Publish Rapid COVID-19 Guidance on Vitamin D (2020). Available online at: https:// www.nice.org.uk/news / article/nice-phe-and-sacn publish-rapid-covid-19-guidance-on-vitamin-d
40. EFSA European Food Safety Authority. Scientific Opinion on the tolerable upper intake level of vitamin D. EFSA Panel on Dietetic Products, Nutrition and Allergies. EFSA J. (2012) 10:2813. doi: 10.2903/ j.efsa.2012.2813
41. Calder PC, Carr AC, Gombart AF, Eggersdorfer M. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients. (2020) 12:1181. doi: 10.3390/nu12041 181
42. Das RR, Singh M, Naik SS. Vitamin D as an adjunct to antibiotics for the treatment of acute childhood pneumonia. Cochrane Database Syst Rev. (2018) 7:CD011597. doi: 10.1002/14651858. CD011597.pub2
43. Norlin AC, Hansen S, Wahren-Borgstrom E, Granert C, Bjorkhem-Bergman L, Bergman P. Vitamin D3 supplementation and antibiotic consumption – results from a prospective, observational study at an immune-deficiency unit in Sweden. PLoS One. (2016) 11:e01 63451. doi: 10.1371/journal. pone. 0163451
44. Siddiqui M, Manansala JS, Abdulrahman HA, Nasrallah GK, Smatti MK, Younes N, et al. Immune modulatory effects of vitamin D on viral infections. Nutrients. (2020) 12:2879. doi: 10.3390/nu12 092879
45. Hewison M Vitamin D and immune function: an overview. Proc Nutr Soc. (2012) 71:50–61. doi: 10.1017/S0029 665111001650
46. Grant WB, Lahore H, McDonnell SL, Baggerly CA, French CB, Aliano JL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID-19 infections and deaths. Nutrients. (2020) 12:988. doi: 10.3390 /nu120 40988
47. Laird E, Rhodes J, Kenny RA. Vitamin D and inflammation: potential implications for severity of Covid-19. Ir Med J. (2020) 113:81.
48. Kara M, Ekiz T, Ricci V, Kara O, Chang KV, Ozcakar L. ‘Scientific Strabismus’ or two related pandemics: coronavirus disease and vitamin D deficiency. Br J Nutr. (2020) 124:736–41. doi: 10.1017/ S0007114520001749
Credits: Derbyshire EJ and Calder PC (2021) Respiratory Tract Infections and Antibiotic Resistance: A Protective Role for Vitamin D? Front. Nutr. 8:652469. doi: 10.3389/ fnut.2021.652469