O. A. Sowunmi1*, P. O. Onifade1 and A. Ogunwale1
1Neuropsychiatric Hospital, Aro, Abeokuta, Ogun State, Nigeria.
ABSTRACT
Earlier studies of Correctional Officers have already shown the relationships between work environment and mental health. However, most have not evaluated the prevalence of specific psychiatric morbidity among officers who work in the prison environment. The aim of this study was to determine the prevalence of DSM-IV/ICD-10 Axis I psychiatric disorders among correctional officials in Abeokuta, Ogun State, Nigeria. A census of all Correctional Officers was conducted at the first stage, during which they were screened for psychiatric morbidity. Those screened positive and 15% of those who were negative were evaluated for definite psychiatric morbidity. The most common mental health disorder was Generalized Anxiety Disorder followed by Major Depressive Disorder, while the least common disorders were Bipolar Disorder (Mania), and Social Phobia. Correctional Officers are at risk of experiencing psychiatry morbidity and as such mental health strategies including education and screening should be integrated into the health management culture of the prison organization for the purpose of prevention and early intervention.
1. INTRODUCTION
A prison is a place for punishment for the behaviour of an individual whose life pattern is not in line with accepted norms, values or behaviours of the society as dictated by the law of the land. The essence of such punishment is for reformation or correction of deviant behaviours and a deterrent to would-be offenders of such laws1. The role of prison officials, among others, includes identifying the causes of the prisoners’ anti-social dispositions, setting in motion mechanisms for their treatment and training for eventual reintegration into society as normal law-abiding citizens after their release from prison. Farkas et al have suggested that the tendency towards professionalism in prison administration has resulted in an ideological shift where prison officers are now expected to perform dual and seemingly conflicting roles of custody and rehabilitation of prison inmates. These conflicting roles have been suggested to impact negatively on the mental health of Correctional Officers 2.
The World Health Organization (WHO) defines mental health as “A state of well-being in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make contributions to his or her community” 3. WHO included the ability to work productively as a measure of health and this can be related to the definition of occupation which refers to a specific chunk of activities in relation to a specific setting and culture 4.
Earlier studies of Correctional Officers have already shown the relationships between work environment and mental health. In Australia, Webster et al 5,6 showed that sleeping pills consumption was higher among Correctional Officers than among the general population and that more prison officers were more vulnerable to psychological distress. In New Zealand, Long et al 6,7 reported that Correctional Officers were more stressed than army personnel and that the degree of psychological distress correlated with the unit the individual served in the workplace. Furthermore, in Great Britain, the study by Rutter & Fielding opined that the following were instrumental in the development of psychological distress: the organization of work 6,8 and relationships with the inmates 6,9. A study conducted in Finland 6,10 also showed that the risk of psychological distress among correctional personnel is linked to the organization of work and to prison characteristics i.e. category and size. Two studies were done in the United States of America on Correctional Officers 6,11,12 revealed the preponderance of occupational over individual characteristics in causing psychological distress.
The aim of this study was to determine the prevalence of DSM-IV/ ICD-10 Axis I psychiatric disorders among correctional officials in Abeokuta, Ogun State, Nigeria.
2. METHODOLOGY
2.1 Study Site and Sample Size
The study was done in Abeokuta the Ogun state capital in Nigeria. It occupies an area of 57.35 sq km with an estimated population of 3,751,140 according to the 2006 population census interim report 13. The prisons used in this study included the following: The Abeokuta prison Oba and the Ibarra Federal Prison.
The Abeokuta prison in Oba was one of the prison formations under the Ogun State Command. It is situated on the east bank of the Ogun River. It had a staff strength of 65 Correctional Officers and a lock-up a population of 545 with an official capacity for one thousand (1000) inmates. The prison at Ibarra had a staff strength of 126. It had a lock-up a population of 562 with an official capacity of 400.
2.2 Study Design
This study is a descriptive, cross-sectional study of psychiatric disorders among Correctional Officers in a prison formation in Abeokuta, Ogun State, Nigeria.
2.3 Data Collection
The study was done in two stages. The first stage involved eliciting participants’ sociodemographic data and screening of participants for psychiatric morbidity using the 28-item version of the General Health Questionnaire (GHQ-28). The second stage involved a clinical interview with the M.I.N.I International Neuropsychiatry Interview-Plus (MINI-PLUS) of all the participants who are GHQ-positive and randomly selected 15% of those who were GHQ – negative.
2.4 Data Analysis
Data were analyzed using the Statistical
Package for Social Science (SPSS version 21) Computer Software. While the prevalence of psychiatric disorders was evaluated after the data were weighted using the Horvitz-Thompson estimator 14:
П = Σ wi yi/ Σ wi
Where П = estimate of prevalence (weighted prevalence).
Σ = “the sum of”.
wi = ith subject’s sampling weight.
yi = 1 (when the ith second stage subject is a ‘true’ case, 0 otherwise).
Further explanation can be found in the work of Dunn et al. 14
2.5 Ethical Consideration
Ethical approval was sought from the Research and Ethics Committee of the Neuropsychiatry Hospital, Abeokuta, and permission was obtained from the management of the different prison formations in Abeokuta Ogun state. Informed consent was obtained from each subject, who was assured of confidentiality. This study had no adverse consequence on the participant physical or otherwise but rather those in need of psychological treatment were assisted by the Prison management to access treatment as advised.
3. RESULTS
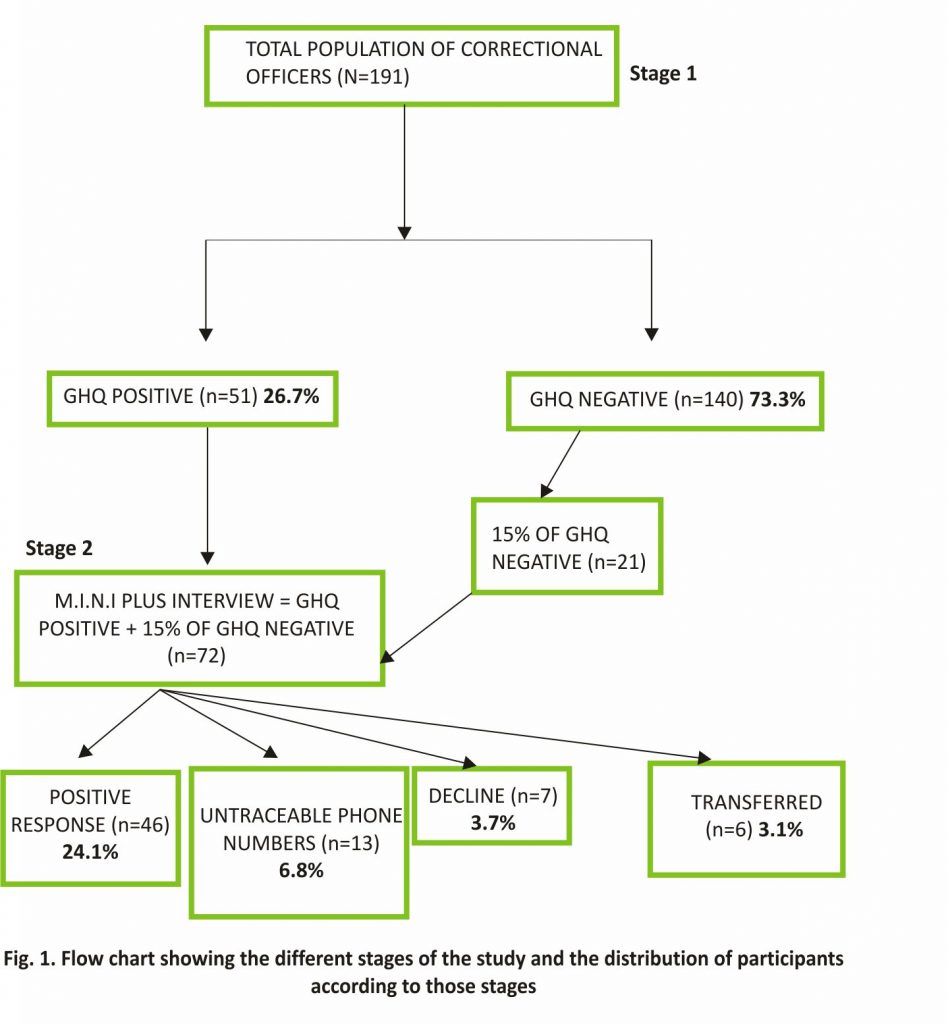
This was a two-stage study. In the first stage, a total of 191 participants completed the General Health Questionnaire version 28 (GHQ-28) and a questionnaire designed to elicit the sociodemographic characteristics of the participants. Out of these 191 Correctional Officers that were surveyed, 51 (26.7%) participants who were GHQ-positive were to be interviewed in the second stage of the study with the Mini International Neuropsychiatric Interview (M.I.N.I PLUS). Also, 21 (15%) of participants who were GHQ negative were randomly selected and were to be interviewed in the second stage. The response rate in the second stage of the study was 64% (n=46). Thirteen (6.8%) participants could not be traced, 7 (3.7%) declined the interview and 6 (3.1%) had been transferred permanently outside Abeokuta prison formation within the 2-week interval of the first and second stage of the study. (See Fig. 1).
3.1 Socio-Demographic Characteristics of Respondents
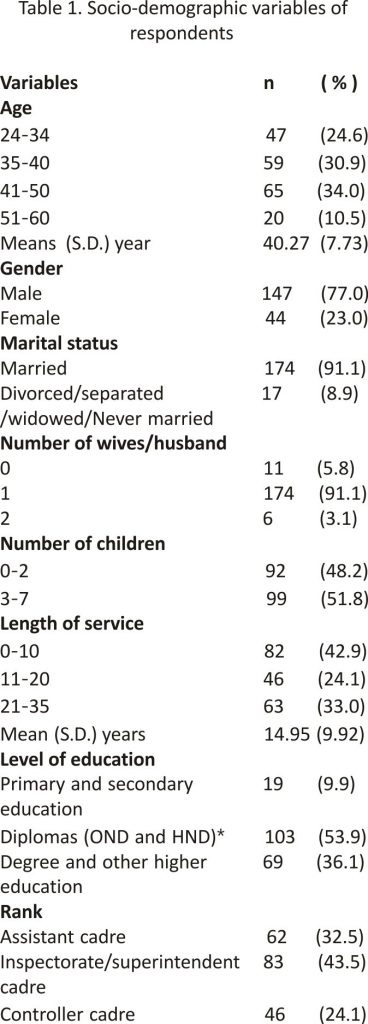
Table 1 shows the socio-demographic characteristics of the participants. The ages of the participants ranged between 24 to 60 years, with a mean of 40.27 years (S.D.±7.73). Most of the participants were in the age bracket of 35-40 years (30.9%), were males 77%, married 91.1%, had one wife/husband (91.1%), and had three or more children 51.8%. The mean length of service was 14.95 years (S.D ± 9.92).
3.2 Specific Psychiatric Disorder
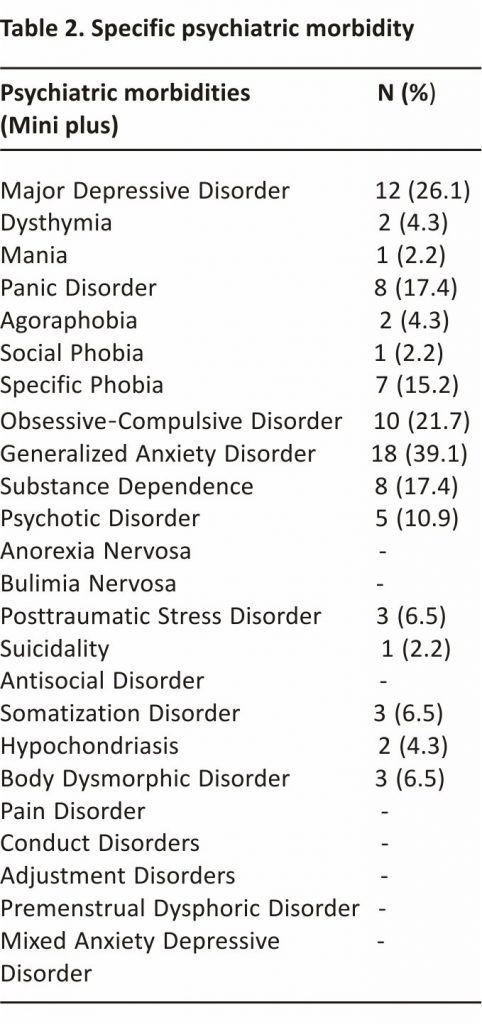
In this study, the most common mental health disorder was Generalized Anxiety Disorder, 18 (39.1%) followed by Major Depressive Disorder 12 (6.3%) while the least common disorders were Bipolar Disorder 1 (2.2%), Social Phobia and Suicidality 1 (2.2%). The remaining specific psychiatric disorders can be found in Table 2.
3.3 Prevalence of Respondents with More Than One Mini-Plus Diagnosis
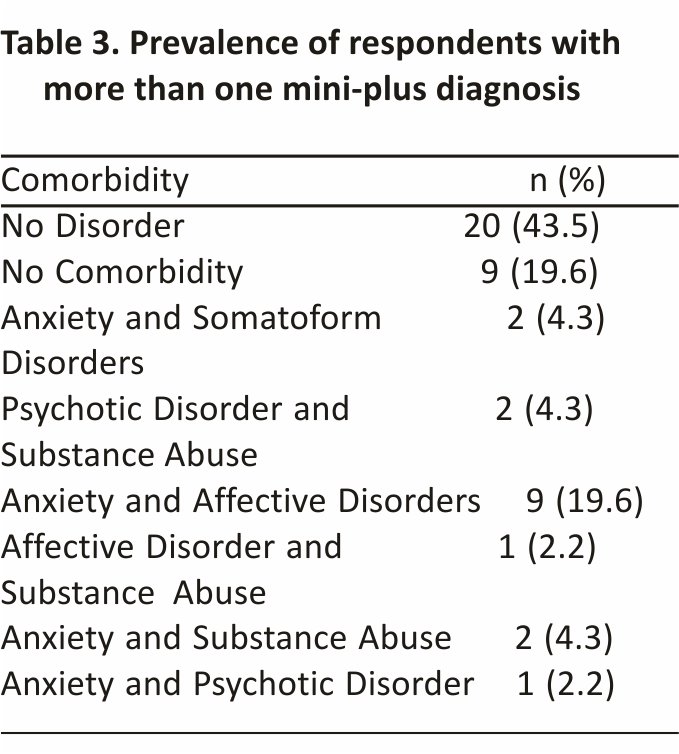
In this study, it was observed that anxiety disorder was the most prevalent (in combination with another psychiatric disorder) comorbid psychiatric morbidity among Correctional Officers. Anxiety and Affective (Depression and Mania) disorders were the most 9 (19.6) comorbidity among Correctional Officers. Other details are highlighted in Table 3.
4. DISCUSSION
4.1 Socio-Demographic Characteristics
The mean age (40.27years) of participants in this study is comparable to that of similar studies conducted in Nigeria among police officers (39.8 years) as well as one study among Correctional Officers in France with a mean age of 37 years 15–17. This may suggest that a predominantly young and middle-aged workforce is desirable for the demands of prison service and perhaps other relevant sections of the criminal justice system.
Furthermore, more than three-quarters of the participants were males, similar to what was reported in a study among Correctional Officers in Edo State, Nigeria 18, This is consistent with the argument of Wells et al, who suggested that traditionally, the prison service is a male-dominated profession in need of aggressive masculine skills 19,20. A French study among Prison Officers also found a preponderance of males 17.
Most of the participants were married while only a tenth was divorced/ separated, widowed or never married. A study among civil servants also reported a comparable percentage of married participants (more than three-quarters) 21. While the number reported in the study among civil servants may not be directly applicable to officers in a correctional environment, an indirect inference may be made since as government employees they could be regarded as public servants as well. Nine out of ten participants had one wife while the remaining one-tenth represented participants that had no wife or those that had more than one wife. This was suggestive of a predominant monogamous setting. The reasons for this predominance maybe because this present study was conducted in the south-western part of the country where Christianity is the predominant religion 22 and monogamy appears to be the normative matrimonial disposition of adherents of the Christian faith. Participants who had two children or fewer were slightly less than half of the survey participants, while more than half (51.8%) had three children or more. This is similar but slightly lower than what was found by Yussuf et al in a study involving a different Nigerian occupational group (bankers) among whom they observed that two-thirds of the participants in their survey had three or more children. The reason may be that it is admirable in Nigerian cultures to have fairly large nuclear families although the trend may be gradually drifting towards a more conservative number of children as found in deeply westernized societies 23,24.
A predominantly monogamous setting might be indirectly suggestive of essentially nuclear family settings which appeared to be the common family type in this study. However, one-third of the participants had five or more dependents.
The reason for this may be that the extended family system could account for the higher number of dependents and is still a common practice in Nigeria. Furthermore, studies among other occupational groups have also shown a third to two-thirds of participants in those studies had five or more dependents subject to their economic status 24–27.
The mean years in service revealed that most individuals had spent more than a decade in service. These findings are similar to those obtained from other studies done among Prison Officers in Ibadan, Oyo state and Edo State where from two-thirds to three-quarters of Prison Officers had spent more than a decade in service15,16,18. This may suggest that the Prison Service provides somewhat stable employment on the one hand, or that Correctional Officers find it difficult to change their career and inadvertently remain on the job, on the other hand, 28.
The Prisons are Federal Government Institutions. Thus, the finding of nine out of ten officers with tertiary education is generally consistent with reports of studies among Federal Government Workers in Nigeria among whom it has been suggested that stable and more financially rewarding employment with the Federal Government is more likely if they possessed a tertiary education 29.
Seven out of ten Correctional Officers were of the junior and middle officers’ ranks. This agrees with figures from an earlier study by Jurik among Prison Officers in the US where nine out of ten of them were either junior or middle-ranked officers 30. A higher proportion of the participants in this study are middle-ranking staff. Previous studies have suggested that the higher proportion of these cadres in the Prison Service is because these officers may be considered the backbone of the workforce since they are the cadres usually called upon to ‘act down’ as well as provide support for the senior officers in their executive and administrative capacity 31.
4.2 Prevalence of Psychiatric Morbidity
Several studies have reported differing prevalence rates of psychiatric morbidities among different occupational groups which were similar to what was found in this study. It was observed that more than a quarter of participants were GHQ positive, with this implying probable psychiatric morbidity. The prevalence of probable psychiatric morbidity among doctors at the University of Benin teaching hospital was reported to be 14% 32. Yussuf et al conducted a number of studies on psychiatric morbidity among workers and found that two out of ten tertiary hospital consultants had probable psychiatric morbidity; about the same proportion was observed to have probable psychiatric morbidity among bank workers in a northern Nigerian setting 24,33. Interestingly, a similar proportion of nursing staff of a Nigerian University Teaching Hospital reported probable psychiatric morbidity 34. In a comparative study also conducted by the same authors, they reported that Resident Doctors had a higher prevalence of probable psychiatric morbidity than Nurses and Consultants while a quarter of Resident Doctors had probable psychiatric disorder 25.
In the main, the findings from this are similar to what was published by Fitzgerald et al in Australia, where over 33% of Correctional Officers had probable psychiatric disorder 35. While it may be said from the foregoing that the rate (26.7%) of probable psychiatric morbidity among the Correctional Officers in this study is comparable to that in some other occupational groups, the rate is nevertheless higher than rates (14%) among doctors in Benin; 18% among Bankers) generally reported in Nigeria. One plausible reason for this slightly higher rate is the impact of the demand that comes with working under pressure within the prison correctional settings and the various forms of danger that the Correctional Officers involved in this study are exposed to and which they are likely to experience on a regular basis 35. However, it is important to note that Fitzgerald et al noted that prison location 36 level of security of the prison37 and respondent prior psychopathology before assumption of work37 as a Correctional Officer may be cofounders which are beyond the scope of this study 35,36.
4.3 Prevalence of Major Depressive Disorder
The weighted lifetime prevalence of major depression among Correctional Officers in this study was 26.1%. This prevalence is however similar to the range reported by most studies (4-30%) which also include military personnel as observed by Cowen et al. 38,39. Prison officers who also have some form of paramilitary training may be exposed to similar stressors as seen among deployed military personnel and this might explain their similarities in terms of the prevalence of Major Depressive Disorder. The cross-national epidemiology of major depression done by Gonzalez et al in the united states of America showed a lifetime prevalence of 14.6% and a 12-month prevalence of 5.5% and that reported among African-American foreign-born by Bromet et al. was 13.4% 16,40,41. The authors opined that Blacks and Latinos appear to have a higher disease burden related to a lack of consistent access to care. In addition, the predominant male gender, an extension of work time without commensurate compensation in the light of the recent security challenges 16 in the country are likely confounders that may have affected the rates observed in this study16. Furthermore, Correctional Officers are more likely to experience loss of life due to jailbreaks and assault from criminals 42. The ban on employment by the Federal government 42 coupled with the inability to protest against poor condition of service 42 and prolonged delay in promotion when compared with other civilian public servants 42 may support a form of learned helplessness42 among Correctional Officers. The above may serve as predisposing, precipitating and perpetuating factors for a depressive disorder in this occupational group.
4.4 Prevalence of Dysthymia
The weighted lifetime prevalence of dysthymia among Correctional Officers was found to be 5.3%. The prevalence rate in this study is however higher than the 4% reported by Alonso et al in six European countries 43. This difference may be driven by cultural factors. Research has suggested that the ‘idiom of distress in the context of mood disorders tend to vary among cultures 44. It is quite possible that the Correctional Officers may be culturally conditioned to reflect emotional distress in less psychological ways such that they might be more prone to report such symptoms as might be suggestive of dysthymia.
4.5 Prevalence of Anxiety and Obsessive-compulsive Disorder
The following anxiety disorders were elicited from the participants in the study: Panic disorder, agoraphobia, social phobia, and specific phobia.
The weighted lifetime prevalence of panic disorder was higher than that reported by Gureje et al (0.2%). The authors conducted their study in the general population, unlike this study that examined only Correctional Officers. In addition to fairly general ‘threats’ in everyday life, Correctional Officers are likely to experience more threatening stimuli in the prison environment. This becomes more relevant with the possibility of their re-deployment to prisons located in states facing the recent wave of insurgency and religious fundamentalism in Nigeria6. The weighted lifetime prevalence of generalized anxiety disorder found in this study was 39.1%. The prevalence of generalized anxiety disorder is higher than the range reported by Gureje et al and Cowen et al which was 4.1% to 5.75% and 0.8% to 6.4% respectively in a general population setting. The high prevalence of generalized anxiety disorder among Correctional Officers may be associated with the increased personal safety concerns that may arise as guards of criminals. In addition, the possibility of jailbreaks 18 which had been worsened by the prevailing political climate in the country may also have contributed to the rate observed among them 18.
The weighted prevalence of specific phobia among Correctional Officers in this study was 15.2%. This was lower than that reported by Guliekin (16.6%) and that reported by Cowen et al. (7% for men and 17% for women) 38,45,46. The difference may be explained by the socio-demographic characteristic such as gender distribution (predominantly female), differential age of onset and cultural differences associated with specific phobia 46. The weighted lifetime prevalence of the obsessive-compulsive disorder in this study was 21.7%. The prevalence of OCD in this study was however higher than that reported by Gureje et al who reported a lifetime prevalence of 0.1% and a 12-month prevalence of 0.1% 45. The prevalence of OCD in this study was also higher than the range reported by Michael et al who reported a range of 0.5-1.6% for lifetime prevalence and 0.5-1.0% for 12-month prevalence 47. Studies 48–51 done among Prison officers have suggested that the higher prevalence of OCD may be explained by the heightened emotions that are related to personnel safety in the prison environment. It is likely that Correctional Officers are more likely to double-check and count prisoners and also lock doors and gates repeatedly in order to ensure safety. Furthermore, obsessive-compulsive traits may be seen as an amiable professional quality which may reduce the chances of been framed or punished for negligence. They also opined that the training and work culture of Prison officers may be a risk factor to the development of psychological disorders which may be related to OCD 18,52
4.6 Prevalence of Mania
The lifetime prevalence of mania among Correctional Officers in this study (2.2%) was comparable to the lifetime prevalence reported by Cowen et al 38. They reported a range of 0.3-1.5% in community surveys. The chronic relapsing nature of manic disorders and the absence of gender difference in mania may explain the similarities observed in these studies.
4.7 Prevalence of Substance Dependence
The weighted lifetime prevalence of substance use disorder in this study was 17.4%. A study among military officers in the United States of America revealed that the prevalence value in this study was higher than 12% reported by the authors. In the same article, it was explained that substance use is associated with cultural acceptability and the amount of pressure that may result from the demand associated with guarding or interacting with criminals 45,53.
4.8 Prevalence of Psychotic Disorder
The weighted lifetime prevalence of a psychotic disorder (schizophrenia, schizoaffective psychosis, and schizophreniform disorder) in this study was 10.9%. A study 54 done among Correctional Officers in the United States of America reported a prevalence of 0.58% which is lower than what was observed in this study. They noted that a relatively lower number of Correctional Officers participated (28%) in their study which when compared with this study was considerably higher (100% and 73% participated in the first and second stage respectively). The instrument used in the study done in America was self-administered while in this study it was interviewer based. Furthermore, because the age of onset for psychotic disorder is lower in males it may explain why Correctional Officers in this study have a higher prevalence 55.
4.9 Prevalence of Posttraumatic Stress Disorder (PTSD)
The weighted lifetime prevalence of Posttraumatic Stress Disorder in this study was 6.5%. Study 56 was conducted in Jos, a city prone to ethno-religious conflicts. These communities had a higher rate (46.1%) when compared to Correctional Officers. This was reasonably so because the prison officers are a largely stable occupational group and may not have experienced a similar traumatic event as seen in Jos 56. Furthermore, the prisons in Abeokuta where the study was done has not experienced any form of crisis in recent times and this might explain the lower rates observed among Correctional Officers in this study. It is likely that the temporal relationship of the traumatic event would affect the proportion of participants that may be observed to have PTSD leaving a sizeable number of participants that have recovered from PTSD.
4.10 Prevalence of Suicidality
The lifetime prevalence of Suicidality (attempt) among Correctional Officers in this study was 2.2%. It was however lower than (2.9%) what was reported in study 57 that looked at the suicide-related outcome in South Africa. In Joe and his coworkers’ submission, they opined that the rates may be related to the effect of apartheid on the particular population that was studied. The period of apartheid was associated with oppression, lack of growth and social opportunity, severe hardship and poor quality of life.
4.11 Prevalence of Somatoform Disorders
The following somatoform disorders were observed among Correctional Officers, namely: somatization disorder, body dysmorphic disorder and hypochondriasis. The lifetime prevalence of Somatization disorder in this study was 6.5%. This was lower than what was observed among teachers in Abeokuta which were 7.38%.16 It appears that teaching is a predominantly female profession was more likely to have respondents who tended to express their psychological distress as a somatoform disorder. This was opined by the author to be a possible reason for the higher rates. It was also noted that eliciting lifetime symptoms will depend on accurate recall of symptoms that may have occurred over 20-30 years. This may have accounted for the lower rate observed in this study.
The lifetime prevalence of hypochondriasis in this study was 4.3%. It was lower than the primary care survey reported by Cowen et al who reported a lifetime prevalence of around 8% 38,58. One of the limitations indicated by the authors is the difficulty in comparing rates around the world. Different instruments have been used with different definitions of hypochondriasis. Moreover, different study sites (e.g. primary health care centres and specialist hospital) along with the method of analysis may have accounted for the discrepancy observed. They also believe that some of the symptoms may have been explained away as medically unexplained symptoms. This may have suggested why a lower rate was observed in this study.
The lifetime prevalence of Body Dysmorphic Disorder (BDD) in this study was 6.5%. This was higher than what was reported (1.7%) in a population-based study in the United States of America 59. Rief et al were of the opinion that self-rating scales might be associated with the less restrictive case definition. This was not the case in this study thus explaining the difference. Moreover, some of the participants had concerns about unattractive body part but did not fulfil the criteria for BDD. In addition, the authors however noted that the prevalence rate varied with the population and that the prevalence also changed within the same population depending on whether a self-administered or clinical interview questionnaire was used. They were of the opinion that clinically administered questionnaire was associated with higher rates 60.
4.12 Prevalence of Psychiatric Comorbidity
The rate of comorbidity among Correctional Officers was higher than what was found among civilians who do not work within the criminal justice system but similar to what was reported among Correctional Officers in the United States 61–66. The prison service may foster a sense of helplessness and this may account for mood and anxiety disorders which were the most prevalent comorbidity in this study. It has been opined that the rigid quasi-military work environment may have an iatrogenic role in the development of anxiety, somatoform and mood disorders 54.
5. CONCLUSIONS AND RECOMMENDATIONS
Despite the usual limitations of cross-sectional studies done with the aid of a questionnaire, our survey corroborated some of the results already reported and enabled us to define the prevalence of psychiatric morbidity among Correctional Officers in Abeokuta Ogun State Nigeria. Mental health preventive strategies including education and screening should be integrated into the health management culture of the organization such that intervention needs to be focused on as early as the screening stage of employment. Tackling work-related mental health issues can be challenging, however, it can also serve as a vehicle for positive change.
This study has shown the burden of psychiatric morbidity and that it may be beneficial to have mental health professionals in the prison system who will be able to screen and plan interventions for officers who may experience mental disorders post-crisis exposure in order to mitigate the effects of such crisis in the short and long term. Finally, it is recommended that future studies consider mental health management intervention and support among Correctional Officers.
CONSENT
As per international standard or university standard, the patient’s written consent has been collected and preserved by the authors.
ETHICAL APPROVAL
As per international standard or university standard, written approval of the Ethics committee has been collected and preserved by the authors.
COMPETING INTERESTS
Authors have declared that no competing interests exist.
REFERENCES
1. Baumer EP, O’Donnell I, Hughes N. The porous prison: A note on the rehabilitative potential of visits home. The Prison Journal. 2009;89: 119–26.
2. Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: A meta-analysis. Occup Environ Med. 2005;62(2):105–12.
3. Herrman H, Jané-Llopis E. The status of mental health promotion. Publ Heal Rev [Internet]. 2012;34(2):1– 21. Available: http://www.publichealthreviews.eu/show/p/109
4. Farias L, Asaba E. “The family knot”: Negotiating identities and cultural values through the everyday occupations of an immigrant family in Sweden. J Occup Sci [Internet]. 2013;20(1):36–47. Available: http://www.tandfonline.com/doi/abs/ 10.1080/14427591.2013.764580
5. Webster IW, Porritt DW, Brennan PJ. Reported Health, lifestyle and occupational stress in prison officers. Community Health Stud. 1983;7(3): 266–77.
6. Sowunmi OA, Onifade PO, Ogunwale A. Psychological disorders and their relationship with job dissatisfaction among correctional officers. Clin Psychiatry [Internet]. 2017;3(1):4-9 Available: http://clinical-psychiatry.imedpub.com/psychological-disorders-and-itsrelationship-with-job-dissatisfactionamong-correctionalofficers.php?aid=19250
7. Long N, Shouksmith G, Voges K, Roache S. Stress in prison staff: An occupational study. Criminology [Internet]. 1986;24(20): 331-45. Available:http://doi.wiley.com/10.1111/j.1745-9125.1986.tb01499.x
8. Rutter DR; Fielding PJ. Sources of occupational stress: An examination of British prison officers. Work Stress. 1988;2(4):291-9.
9. Launay G, Fielding PJ. Stress among prison officers: Some empirical evidence based on self-report. Howard J. 1989;28(2):138-47.
10. Shiri R, Martimo K, Miranda H, Ketola R, Kaila- L, Liira H, et al. Stress in work: Conceptual analysis and a study on prison personnel. Scand J Work Environ Health. 2016;6(1): 124-200.
11. Gerstein LH, Topp CG, Correll G. The role of the environment and person when predicting burnout among correctional personnel. Crim Justice Behav. 1987;14(3):352 -69.
12. Whitehead JT, Lindquist CA. Correctional Officer job burnout: A path model. J Res Crime Delinq [Internet]. 1987; 23(1):23-42. Available:http://hjb.sagepub.com.proxy.lib. umich.edu/content/9/2/183.full.pdf+html%5Cnhttp://hjb.sagepub.com/cgi/doi/10.1177/07399863870092005
13. Okodua M, Adeyeba OA, Tatfeng YM, Okpala HO. Age and sex distribution of intestinal parasitic infection among HIV infected subjects in Abeokuta, Nigeria. Online J Heal Allied Sci. 2003;2(4):20-4.
14. Dunn G, Pickles A, Tansella M, Vázquez-Barquero JL. Two-phase epidemiological surveys in psychiatric research: Editorial. British Journal of Psychiatry. 1999;174:95-100.
15. Aremu AO. Impact of some demographic variables on job satisfaction of women police in Ibadan, Nigeria. Gend Behav. 2006;4(1) :736.
16. Oyetola S. Cross-sectional survey of job satisfaction and psychiatric morbidity among secondary school teachers in Abeokuta, Ogun State, Nigeria. Dissertation submitted to the West African College of Physicians, Faculty of Psychiatry in partial fulfilment of the req; 2011.
17. Goldberg P, David S, Landre MF, Goldberg M, Dasse S, Fuhrer R. Work conditions and mental health among prison staff in France. Scand J Work Environ Health. 1996;22(1):45-54.
18. Imhonde H. The jailer or the jailed: Stress and prison workers in Nigeria. Curr Res J Soc Sci [Internet]. 2010;2(2):65-8. Available: http://www.doaj.org/doaj?func=abstract&id=521545
19. Wells T, Colbert S, Slate R. Gender matters: Differences in State probation officer stress. J Contemp Crim Justice. 2006;22(1):63–79.
20. Griffin ML. Correctional officers’ perceptions of equitable treatment in the masculinized prison environment. Criminal Justice Review. 2005;30:189-206.
21. Paul EP, Phua SK. Lecturers’ job satisfaction in a public tertiary institution in Singapore: Ambivalent and non-ambivalent relationships between job satisfaction and demographic variables. J High Educ Policy Manag. 2011; 33(2):141-51.
22. Rosalind IJ. Charismatic/ Pentecostal Appropriation of Media Technologies in Nigeria and Ghana Author (s): Rosalind IJ. Hackett Published by: BRILL Stable J Relig Africa. 2011;28:258-77. Available: http://www. jstor.org/stable/1581571.
23. Wang JL, Lesage A, Schmitz N, Drapeau A. The relationship between work stress and mental disorders in men and women: Findings from a population-based study. J Epidemiol Community Health. 2008;62(1): 42-7.
24. Yussuf AD. Risk factors for psychiatric morbidity among bank workers in a northern city of Nigeria. South African J Psychiatry [internet]. 2005;11(2): 63-8. Available: http://www.scopus.com/inward/record. url?eid=2-s2.0-27744556258&partnerID=
40&md5=874c7accc7fea480d90815270ae bf8c925.
25. Yussuf AD, Kuranga SA, Balogun OR, Ajiboye PO, Buhari OI. Comparative psychiatric morbidity among three groups of health professionals in a Nigerian tertiary health institution. Nigerian Journal of Psychiatry. 2008; 5:31-7.
26. Yussuf AD, Balogun OR, Kuranga SA. Prevalence and risk factors for psychiatric morbidity among tertiary hospital consultants in Nigeria. South African J Psychiatry [Internet]. 2006; 12(2):26-36. Available: http://www. scopus.com/ inward/record.url?eid=2-s2.0-3384648 2001&partner ID=tZOtx3y1
27. Ugwa EA, Muhammad LM, Ugwa CC. Job satisfaction among nurses and doctors in a tertiary hospital in a cross-sectional study. Int J Hosp Res. 2014;3(1):11-8.
28. Stansfeld S, Candy B, Psychosocial B. Finnish institute of occupational health Norwegian national institute of occupational health a meta-analytic and mental review work environment psychosocial. Scand J Work Environ Health. 2014;32(6): 443-62.
29. Dabalen A. Labor market prospects for university graduates in Nigeria. High Educ Policy. 2001;14(2):141-59.
30. Jurik NC. Striking a balance: Female correctional officers, gender role stereotypes and male prisons. Social Inq. 1988;58(3):291-305.
31. Brown J, Campbell E. Sources of occupational stress in the police. Work & Stress. 1990;4:305-18.
32. Ofili AN, Asuzu MC, Isah EC, Ogbeide O. Job satisfaction and psychological health of doctors at the University of Benin Teaching Hospital. Occup Med (Chic Ill). 2004;54(6): 400-3.
33. Yussuf AD, Balogun OR, Kuranga SA. A survey of psychiatric morbidity and the risk factors among chief executives of tertiary health institutions in Nigeria. Nigerian Journal of Psychiatry. 2007;4.
34. Yussuf AD, Kuranga SA, Balogun OR, Ajiboye PO, Buhari OIN. Psychiatric morbidity among the Nursing staff of a University Teaching Hospital in Nigeria. Niger J Psychiatry. 2007; 5(1):45-9.
35. Morrison D. The effects of job design on physical and mental health among prison officers. Int J Emerg Ment Health. 2007; 7(1):1-15.
36. Schaufeli WB, Peeters MCW. Job Stress and burnout among correctional officers: A literature review. Int J Stress Manag [Internet]. 2000;7(1):19-48. Available: http://www. scopus.com/inward/record.url?eid=2-s2.0-0034414891&partnerID=40&md5=a 31306b6e5e3428aeb0f53e3c4f03b89
37. Dunne MP, Morrison D. Health, stress and job satisfaction in prison officers. J Occup Heal Saf – Aust New Zeal [Internet]. 1991; 7:49-58. Available: http://ovidsp.ovid.com/ ovidweb.cgi?T=JS&CSC=Y&NEWS=N&PAGE=fulltext&D=emed2&AN=1991119667%5Cnhttp://openurl.man.ac.uk/sfxlcl3?sid=OVID:embase&id=pmid:&id=doi:&issn=0185-6409&isbn=&volume=7&issue=1&spage =49&pages=49-58&date=1991&title= Journal+of+Occupational+
38. Philip C, Paul H, Tom B. Shorter oxford textbook of psychiatry. 6th ed; 2012.
39. Gadermann AM, Engel COLCC, Naifeh JA, Nock MK, Petukhova M, Santiago LPN, et al. Prevalence of DSM-IV major depression among U.S. military personnel: Meta-analysis and simulation. Mil Med. 2012;177 (8):47.
40. Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Crossnational epidemiology of DSM-IV major depressive episode. BMC Med [Internet]. 2011;9(1):90. Available:http://www. biomedcentral.com/1741-7015/9/90
41. González HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res. 2010;44(15):1043-51.
42. Seligman MEP, Csikszentmihalyi M. Positive psychology: An introduction. American Psychologist. 2000;55:5-14.
43. Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Prevalence of mental disorders in Europe: Results from the European study of the epidemiology of mental disorders (ESEMeD) project. Acta Psychiatr Scand. 2004;109 (420) :21-7.
44. Kirmayer LJ, Groleau D. Affective disorders in cultural context. The Psychiatric Clinics of North America. 2001;24:465-478.
45. GUREJE O. Lifetime and 12-month prevalence of mental disorders in the Nigerian survey of mental health and wellbeing. The British Journal of Psychiatry. 2006;188:465–71.
46. Gültekin BK, Dereboy IF. The prevalence of social phobia, and its impact on quality of life, academic achievement, and identity formation in university students. Turk Psikiyatri Derg [nternet]. 2011;22(3):150-8. Available:http://www.ncbi.nlm.nih.gov/pubmed/21870304
47. Michael T, Zetsche U, Margraf J. Epidemiology of anxiety disorders; 2007.
48. Stack SH. Prison officers “facing threats on daily basis”. Irish Indep. 2007;13(3):6-7.
49. Triplett R, Mullings JL, Scarborough KE. Work-related stress and coping among correctional officers: Implications from organizational literature. J Crim Justice. 1996;24(4):291-308.
50. Adebisi KS, Oyewo oyekunle oluseye. Prisons and security challenges in a democratic Nigeria. Reserch Humanit Soc Sci. 2015;5(6):124-30.
51. Lambert EG. The Impact of job characteristics on correctional staff members. The Prison Journal. 2004;84:208-27.
52. Orakwe IW. The origin of prison in Nigerian. Punishment Soc. 2012;9(3):1-6.
53. Bray RM, Pemberton MR, Lane ME, Hourani LL, Mattiko MJ, Babeu LA. Substance use and mental health trends among U.S. military active duty personnel: key findings from the 2008 DoD Health Behavior Survey. Mil Med. 2010;175(6):390-9.
54. Tartaglini AJ, Safran DA. A topography of psychiatric disorders among correction officers. J Occup Environ Med. 1997;39(6): 569-73.
55. Perälä J, Suvisaari J, Saarni SI, Kuoppasalmi K, Isometsä E, Pirkola S, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007;64(1): 19-28.
56. Tagurum YO, Chirdan OO, Obindo T, Ayotunde BD, Olumide AT, Ibrahim HZ, et al. Prevalence of violence and symptoms of post-traumatic stress disorder among victims of ethno-religious conflict in Jos, Nigeria. J Psychiatry. 2015;18(1):14-138.
57. Joe S, Stein DJ, Seedat S, Herman A, Williams DR. Non-fatal suicidal behaviour among South Africans. Soc Psychiatry Psychiatr Epidemiol. 2008;43(6):454-61.
58. Gureje O, Simon GE, Ustun TB, Goldberg D. Somatization in cross-cultural perspective: A world health organization study in primary care. Am J Psychiatry. 1997;154(7):989-95.
59. Rief W, Buhlmann U, Wilhelm S, Borkenhagen A, Brähler E. The prevalence of body dysmorphic disorder: A population based survey. Psychol Med. 2006;36(6):877-85.
60. Grant JE, Phillips KA. Recognizing and treating body dysmorphic disorder. Annals of Clinical Psychiatry. 2005;17:205-10.
61. Cosoff SJ, Hafner RJ. The prevalence of comorbid anxiety in schizophrenia, schizoaffective disorder and bipolar disorder. Aust N Z J Psychiatry. 1998;32(1):67-72.
62. de Waal MWM, Arnold IA, Eekhof JAH, van Hemert AM. Somatoform disorders in general practice: Prevalence, functional impairment and comorbidity with anxiety and depressive disorders. Br J Psychiatry .2004;184:470-6.
63. Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders on alcohol and related conditions. Arch Gen Psychiatry. 2006;61(2):807-16.
64. Merikangas KR, Mehta RL, Molnar BE, Walters EE, Swendsen JD, Aguilar-Gaziola S, et al. Comorbidity of substance use disorders with mood and anxiety disorders: results of the International Consortium in Psychiatric Epidemiology. Addict Behav [Internet]. 1998;23(6):893-907. Available:http://www. ncbi.nlm.nih.gov/pubmed/9801724
65. Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorder with alcohol and other drug abuse. J Am Med Assoc. 2014;264(19):2511-8.
66. Regier DA, Rae DS, Narrow WE, Kaelber CT, Schatzberg AF. Prevalence of anxiety disorders and their comorbidity with mood and addictive disorders. Br J Psychiatry. 1998; 173 (Suppl 34):24-8.
Credit: Sowunmi, O.A., Onifade, P.O., and Ogunwale, A. (2018). Lifetime Prevalence of Psychiatric Disorders among Correctional Officers in a Prison Formation in Abeokuta Ogun State Nigeria. International Neuropsychiatric Disease Journal, 11(2): 1-12.
DOI: 10.9734/INDJ/2018/40900