NI Ugwu1, CJ Uneke2
1 Department of Haematology and Immunology, Faculty of Clinical Medicine, Ebonyi State University,
Abakaliki, Nigeria
2 Directorate of Research, Innovation and Commercialisation, Ebonyi State University, Abakaliki, Nigeria
Correspondence Address: Dr. N I Ugwu
Department of Haematology and Immunology, Faculty of Clinical Medicine, College of Health Sciences, Ebonyi State
University, Abakaliki Nigeria
Abstract
Anemia in pregnancy is a public health problem in Nigeria and it is more than likely that iron deficiency is the major cause. This study aimed to review relevant publications in order to summarize the prevalence of iron deficiency anemia, risk factors associated with iron deficiency, anemia in pregnancy as well as factors associated with compliance to routine iron therapy. MEDLINE Entrez PubMed search was performed in August 2017 and studies that investigated iron deficiency anemia in pregnancy in Nigeria from 1968 to 2017 were sought. Search keywords included “iron deficiency anemia, pregnancy, Nigeria.” Only studies that provided information on the prevalence of iron deficiency anemia, risk factors associated with iron deficiency anemia and risk factors associated with compliance to routine iron therapy in pregnancy in Nigeria were eligible and were selected. Inclusion criteria were original scientific investigations, not reviews, studies conducted in Nigeria between 1968 and 2017 and studies written in the English language. A total of six relevant studies that fulfilled the study inclusion criteria were identified out of 36 studies found. All the studies reported a high prevalence of iron deficiency anemia among pregnant women and risk factors associated with iron deficiency anemia in pregnancy include multiparity, third trimester of pregnancy, and low socioeconomic status. Risk factors associated with noncompliance to routine iron therapy include poor utilization of antenatal services, low educational attainment, distance to a health facility, single or teenage pregnancy, increasing age of the pregnant women, and living in the rural areas. The prevalence of iron deficiency anemia among pregnant women was reported to be high. Awareness creation and education on the importance of family planning and proper utilization of antenatal care services should be encouraged. There should be economic empowerment of women, provision of health facilities to areas where they are absent to encourage early booking and utilization of antenatal care services.
Keywords: Anemia, iron deficiency, pregnancy
Introduction
Anemia is the commonest hematologic disorder that occurs in pregnancy and is a public health problem particularly in most of the developing countries, as it significantly contributes to an increase in maternal and perinatal morbidity and mortality.1 It is a condition of low circulating hemoglobin (Hb) in which concentration has fallen below a threshold lying at two standard deviations below the median of a healthy population of the same age, sex, and stage of pregnancy causing decreased oxygen-carrying capacity in a pregnant woman.2 This reduced oxygen-carrying capacity results in reduced oxygen supply both to the mother and the developing baby. In developing countries, it is a cause of serious concern as, besides many other adverse effects on the mother and the fetus, it contributes significantly to high maternal mortality.3 It increases the risk of preterm delivery and postpartum maternal infections.4 Globally, more than 2 billion people suffer from anemia; the most common cause being an iron deficiency.5 While WHO defines anemia in pregnancy as hemoglobin level of less than 11 g/dL (or hematocrit less than 33%),6 value of less than 10 g/dL is commonly used in developing countries including Nigeria.7 It has been shown that no significant harm is encountered in the fetus until the hemoglobin concentration drops to less than 10 g/dL. The Center for Disease Control uses hemoglobin concentration of less than 11 g/dL in first and third trimesters and hemoglobin concentration less than 10.5 g/dL in the second trimester.8
Anemia is underreported in most developing countries even though it is one of the most prevalent public health problems and has serious consequences for national development.9 Iron deficiency causes approximately 50% of all anemia (but the proportion varies among population groups and in different areas), and almost a million deaths a year; three-quarters of the deaths occur in Africa and Southeast Asia.10,11 Although more prevalent in less-resourced countries, women from developed countries are also affected. Women from both rural and urban areas are vulnerable.12 A large number of women from less-resourced countries embark upon pregnancy with frank iron deficiency anemia and/or depleted iron stores. Anemia is the major contributory or sole cause in 20–40% of maternal deaths.13
Iron deficiency is the most common nutritional deficiency in the world and accounts for 75% of all types of anemia in pregnancy.6 It is due to the fact that diet in pregnancy is insufficient to supply iron requirements. It has a high prevalence in developing countries, but it is also relevant in developed countries where other nutritional disorders have been almost eliminated. The cause of iron deficiency anemia is usually inadequate dietary intake (especially in adolescent girls), a previous pregnancy, and normal recurrent loss of iron in menstrual blood (which approximates the amount normally ingested each month and, thus, prevents iron stores from building up).6
During pregnancy, there is a physiological hemodilution, with a peak during 20–24 weeks of gestation.14 It is well established that there is a physiological drop in hemoglobin in the mid-trimester. This physiological drop is due to the higher increase in plasma volume (50%), compared with red blood cell mass (30%) during pregnancy. This physiological process produces relative hemodilution, helping the blood circulation in the placenta.15 In addition, during pregnancy, iron deficiency is relatively common because of the increased iron demand with a mean iron requirement of 4.4 mg/day.16 Because many women start pregnancy with poor or depleted iron stores, the amount of iron absorbed from the diet, together with that mobilized from stores, is usually insufficient to meet the maternal demands imposed by pregnancy.16
Nigeria has a high maternal mortality rate and anemia is a major contributor. Iron deficiency is the commonest cause of anemia in pregnancy.17 Various studies have assessed the prevalence and risk factors associated with iron deficiency anemia in pregnancy in Nigeria but none has systematically summarized such studies.3,12 The aim of this review was to summaries the prevalence of iron deficiency anemia in pregnancy in Nigeria and to identify the factors associated with iron deficiency anemia as well as factors associated with compliance to routine iron therapy.
Materials and Methods
A MEDLINE Entrez PubMed search was performed in August 2017 and studies published in English which investigated iron deficiency anemia in pregnancy in Nigeria, risk factors associated with iron deficiency anemia as well as factors associated with compliance to routine iron therapy were sought. PubMed was searched for studies from Nigeria undertaken from 1968 to 2017. The following were the search strategies/ keywords used: “iron deficiency anaemia, pregnancy, Nigeria,” which yielded 36 publications as in August 2017.
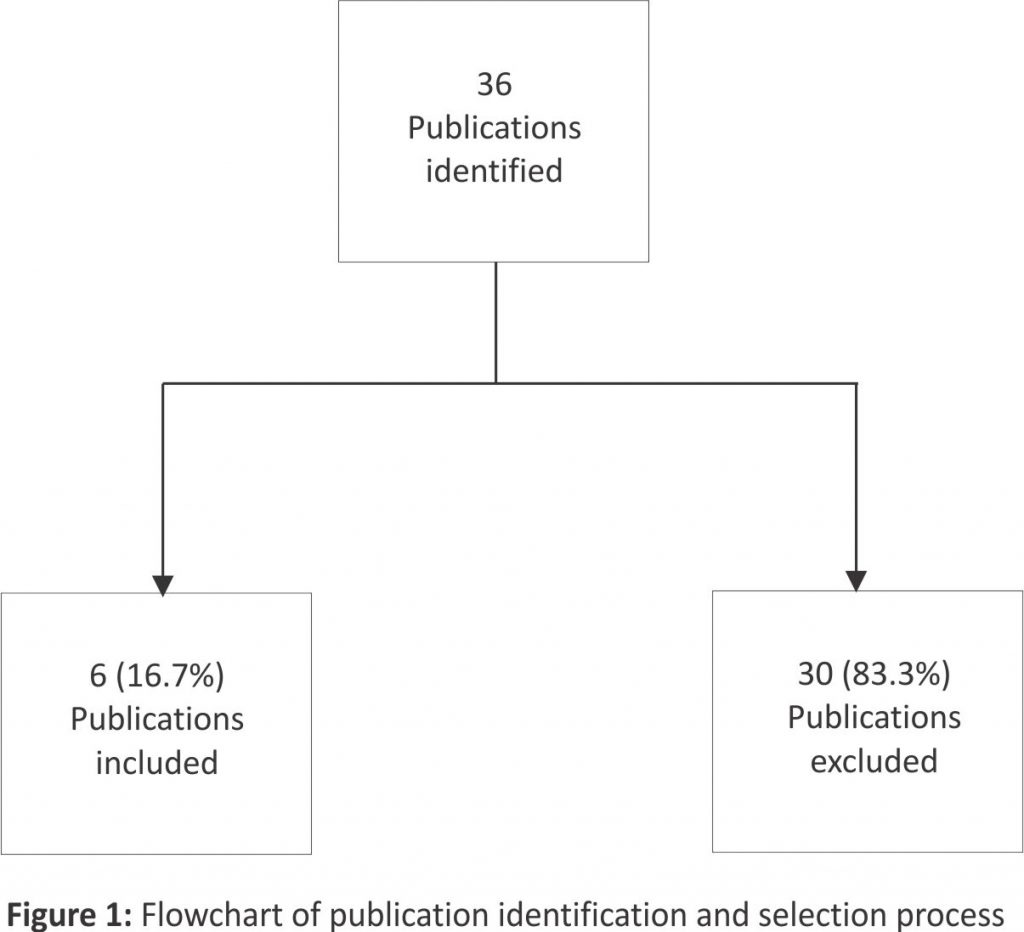
All the publications (36) found were subjected to the study inclusion criteria in order to select the publications which addressed the issue in question as well as met the study objectives. The following study inclusion criteria were used: i) studies conducted in Nigeria between 1968 and 2017. ii) Original scientific investigations, not reviews. iii) Studies conducted which determined the prevalence of iron deficiency anemia in pregnancy, risk factors associated with iron deficiency anemia as well as factors associated with compliance to routine iron therapy. iv) Studies written in the English language. Studies that did not meet these criteria were excluded. Following these processes, six publications were noted to have met the study inclusion criteria and were selected for the review [Figure 1].
Subsequently, the references of all the resulting six publications were hand-searched for additional studies and information relevant to the review. Publications that did not completely fulfill the study inclusion criteria but adjudged to contain vital information necessary for the narrative aspect of the review were selected and used accordingly. The selected publications were then grouped according to the following: author(s)/year of publication, a state where the research took place, study design, evidence generated/ outcome from the study, and policy implication of the study including the recommendations.
Results
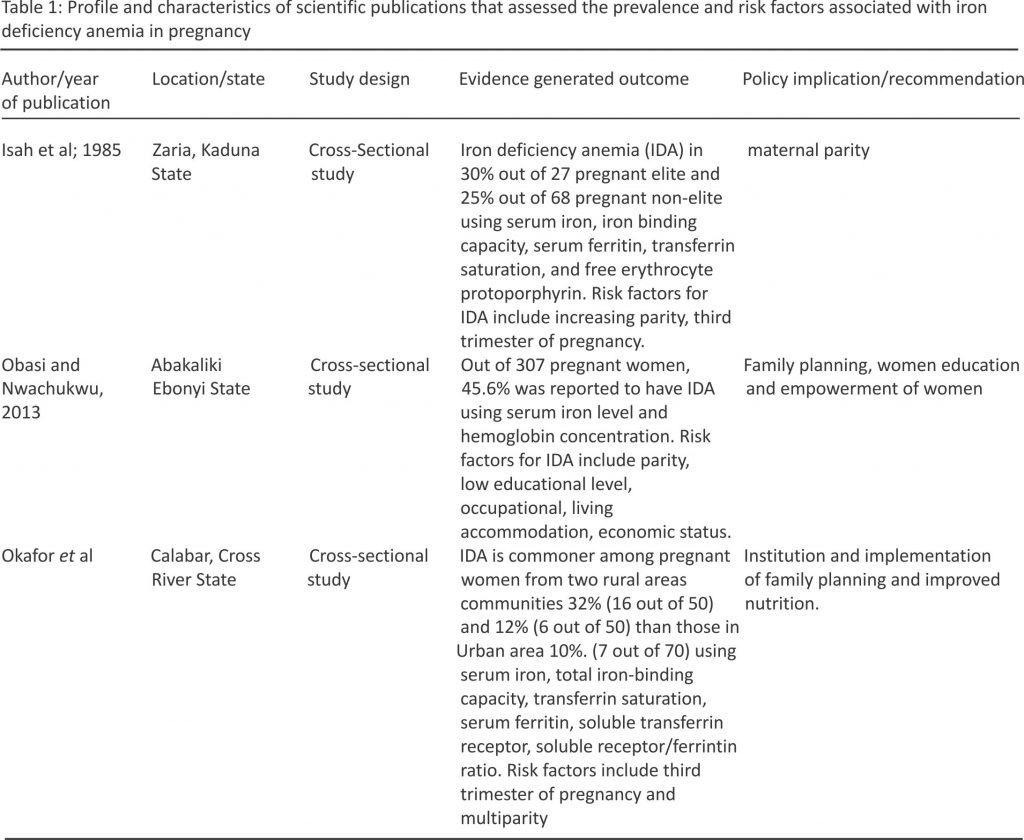
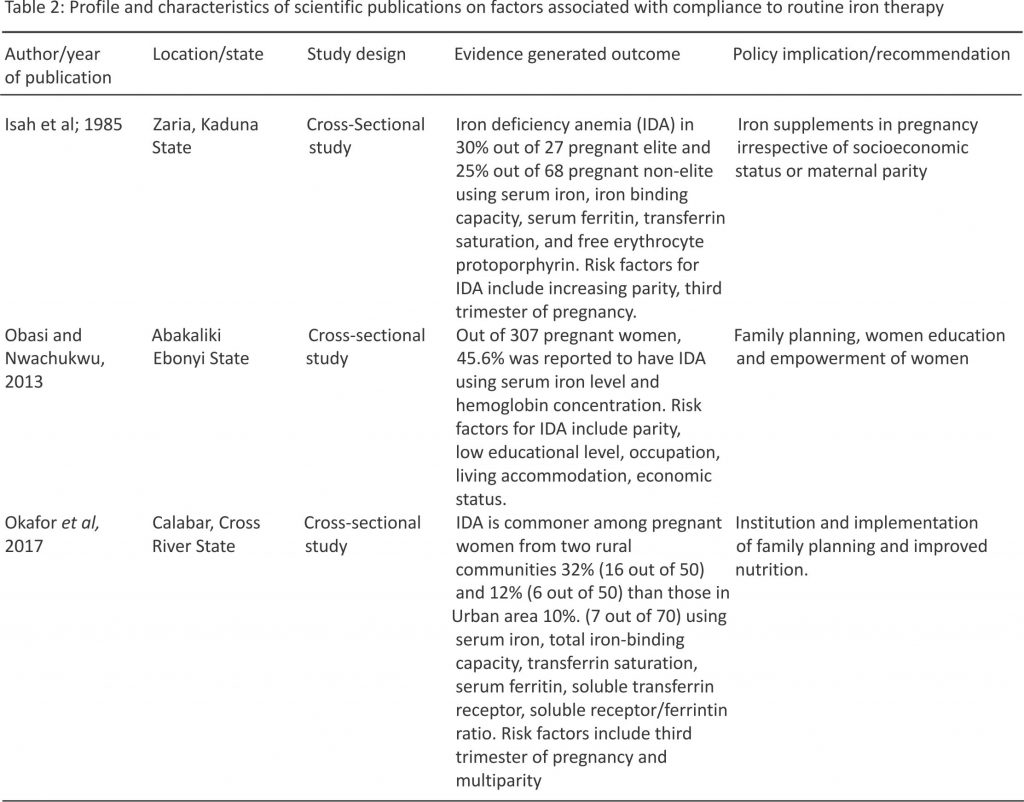
The six studies identified to have met the study inclusion criteria were used for this review. The outcomes of the review are presented in this chapter using tables. For the purpose of ease of presentation and discussion, the publications were categorized into two according to the health issue addressed in the study [Table 1] and [Table 2].
Prevalence and risk factors for iron deficiency anemia in pregnancy
From the search, three out of the six scientific publications (50%) retrieved reported on the prevalence and/or risk factors associated with iron deficiency anemia in pregnancy [Table 1]. The prevalence of iron deficiency anemia was reported to be high, ranging from 25% to 45.6%. Risk factors associated with iron deficiency anemia include multiparity, third trimester of pregnancy, low educational level, and low economic status [Table 1].
Factors associated with compliance with routine iron therapy
[Table 2] presents three (50%) out of the six identified scientific publications (Onyeneho et al., 2016; Dairo and Lawovin, 2006; Adanikin et al., 2015) that reported on the risk factors associated with poor compliance with routine iron therapy. Risk factors reported include poor utilization of antenatal care services, low educational attainment, distance to a health facility, single and teenage pregnancy, and age of the pregnant woman [Table 2]
Discussion
The findings of this review showed that there is a high prevalence of iron deficiency anemia among pregnant women in Nigeria. All the studies reviewed reported certain risk factors associated with iron deficiency anemia in pregnancy. Out of the total of 36 publications found from the MEDLINE search related to iron deficiency anemia in pregnancy in Nigeria, only six (16.7%) fulfilled the inclusion criteria. The implication of this finding suggests that an inadequate amount of research relevant to iron deficiency anemia in pregnancy has been undertaken in Nigeria. This may be due to less attention given to nutrition in pregnancy.
Maternal mortality ratio (MMR) remains high in Nigeria and other countries in sub-Saharan Africa despite a substantial reduction in global trends of maternal deaths.18 Anemia has been implicated as a major contributor to the high maternal mortality rate in Nigeria and other developing countries.19,20,21 The prevalence of anemia in pregnancy varies considerably because of the differences in socioeconomic conditions, lifestyles, and health-seeking behaviors across different cultures.22 Anemia in pregnancy is a common problem in Nigeria with iron deficiency anemia as the commonest cause.23 This review has shown evidence that the prevalence of iron deficiency anemia among pregnant women in Nigeria is still high, ranging from 25% to 45.6%.12,24,25 Nutritional deficiencies resulting in anemia are often worsened by the additional nutrient demands associated with fetal growth.
Risk factors associated with iron deficiency anemia in pregnancy include multiparity, third trimester of pregnancy, and low socioeconomic status (low educational attainment, no occupation, poor living condition). According to Okafor et al. and Isah et al., multiparity is an important risk factor associated with iron deficiency anemia.26,27 Pregnancy consumes a lot of iron, hence, too frequent pregnancies within short intervals will result in iron deficiency.28 The gestational iron demand is 3–4 folds the requirement of the nonpregnant women.29 Although it can be mobilized from the maternal stores to meet this requirement, women in general, are found to have low iron stores probably due to the monthly loss of blood in menstruation.30 Once these stores are depleted, the mother will develop iron deficiency.31 A deficiency of iron causes a reduction in the rate of hemoglobin synthesis and can result in iron-deficiency anemia.32 Reducing the total number of pregnancies, and increasing the time interval between pregnancies will contribute to the control of iron deficiency anemia in women. Family planning and child spacing will reduce iron demand in the woman with resultant prevention of iron depletion, iron deficiency anemia, and its consequences.
Another risk factor reported to be associated with iron deficiency anemia in pregnancy is the third trimester of pregnancy.26,27 During pregnancy, there is an increase in both red cell mass and plasma volume to accommodate the needs of the growing uterus and fetus. The plasma volume increases more than the red cell mass leading to a fall in the concentration of hemoglobin in the blood.33 This drop in hemoglobin concentration decreases the blood viscosity and this enhances the placental perfusion providing a better maternal-fetal gas and nutrient exchange.34 This physiological process occurs as the pregnancy progresses and utilizes iron, further worsening the anemia in the third trimester of pregnancy. The dilution of blood in pregnancy is a natural process and starts approximately at the 8th week of pregnancy and progresses until the 32nd to 34th week of pregnancy.35 In addition, there is a marked demand for extra iron during pregnancy especially in the second half of pregnancy.36 Therefore, the physiological anemia is due to the combined effect of hemodilution and negative iron balance. Although menstruation-related iron losses are reduced to nil during pregnancy, additional iron is nevertheless required for the fetus, the placenta, and the increased maternal blood volume. This amounts to approximately 1000 mg of iron over the entire pregnancy.37 Requirements during the first trimester are relatively small, 0.8 mg per day, but rise considerably during the second and third trimesters to a level of 6–7 mg per day.38
Low socioeconomic factors (such as low educational level, unemployment, and poor living accommodation) were also reported as risk factors for the development of iron deficiency anemia in pregnancy.12 Anemia serves as an indicator of a socioeconomic disadvantage because it is inversely related to the socioeconomic status of households especially in developing settings.39 Individuals with low socioeconomic status are at a higher risk of exposure to anemia and its sequelae.40 The majority of the women with iron deficiency anemia have no occupation as they were housewives with little or no official income.12 This may bring about poor nutritional status among pregnant women as they have low purchasing power and hence low access to better nutrition and better health conditions. In addition, pregnant women are expected to pay for the iron tablets and other medications. Evidence from the review also suggests that women who lack money limit their choice and uptake of iron.12 Opportunities should be created for women’s empowerment.
Closely related to no occupation is low educational attainment which was also reported as a risk factor for iron deficiency anemia. It was reported that the majority of the women with iron deficiency anemia had no formal education or primary education which impacts their economic status.12 It is a common belief that more enlightened women would secure a better job, have a better living condition, and keep better hygienic practices; hence, lower incidence of iron deficiency anemia possibly due to better nutrition as well as reduced chances of parasitic infections, already found to be common in this population.41
Despite the efforts to reduce iron deficiency anemia in pregnancy by administering iron tablets to be taken routinely in pregnancy, this review has also shown that uptake of routine iron by pregnant women is suboptimal. Factors reported affecting routine iron therapy in pregnancy include non-utilization of antenatal care services, low educational attainment, closeness to a health facility, single and teenage mothers.42,43
The use of antenatal care services was reported to be associated with compliance with routine iron therapy. Women who use antenatal care services complied more than those who did not use antenatal care services.43 This is not surprising considering the fact that using antenatal care services exposes women to a lot of benefits. Antenatal clinics offer a lot of services including health education. Health education was demonstrated to be valuable as pregnant women who attend antenatal care were enlightened on the need for routine iron therapy, good nutrition, dispel misconceptions and harmful practices. Moreover, during antenatal care, iron tablets are usually administered to them in addition to other routine drugs and they are usually encouraged to take them to prevent iron deficiency anemia.44
Another factor reported to be associated with compliance to routine iron uptake is the distance to a health facility as those who live close to a health facility tend to utilize antenatal services with better compliance to routine iron therapy than those who live far away.42 Generally, distance has been identified as an important barrier to the use of antenatal care services especially in rural areas.45,46 Distance from a health facility is linked to other factors such as availability and cost of transport. Therefore, a distance far away from a health facility may imply some transportation costs and difficulty accessing health care.
Educational status was also reported as a factor associated with compliance with routine iron therapy among pregnant women. Pregnant women who had secondary education and above were reported to comply more than those who had no formal education or had primary education.42 The finding is supported by other studies done on factors that affect routine iron therapy in pregnancy.47,48 This might be due to the fact that education would increase women’s access to information about iron deficiency anemia and ways to overcome it. In addition, it might also be associated with the fact that educated women have a greater ability to stick to health care advice which is beneficial for both the mother and child.
Findings from this review also reported that living in the rural areas are associated with noncompliance to routine iron therapy.43 Pregnant women who reside in urban areas complied more than those who live in rural areas. This may be because living in urban areas facilitates easier access to a health facility due to easier transportation and, therefore, easy access to iron and other supplements which are usually given as part of antenatal services.
Poor compliance with routine iron therapy was also reported to be more with single and teenage mothers.43 Previous studies have also shown that compliance with routine iron therapy in pregnancy is poor among adolescents.49 The reason for low compliance among adolescent girls could be due to lack of knowledge regarding their hemoglobin status and the usefulness of iron in building up their hemoglobin level.
Increasing age above 30 years was also found to be associated with poor compliance with routine iron therapy during pregnancy.43 Other studies have also reported similar findings.49,50 This could be due to the fact that most of the youngest women are likely to be first-time mothers, hence, more keen to adhere to the advice given on routine iron therapy to ensure the best maternal and fetal outcome. Women who are older are likely to have been pregnant before, may also have experienced side effects of iron before and were, therefore, hesitant to take iron tablets. They may take for granted advice during pregnancy especially if they have not experienced any difficulties with the previous pregnancy.50 This shows the need to persistently teach pregnant women the importance of adhering to routine iron therapy in their subsequent pregnancies.
Some of the reasons given by noncompliant pregnant women for not adhering to routine iron uptake were forgetfulness, fear of side effects (gastrointestinal upsets, constipation, and nausea), and fear of harm to the baby.49 The finding of this study is supported by other studies.51,52 A possible explanation for forgetfulness maybe because most pregnant women might be tired after the day’s activities. The majority of women who do not comply with routine iron therapy have a misunderstanding that consuming iron tablets during pregnancy may cause harm to their baby.53 Proper counseling will help to correct superstitious belief about taking iron tablets among pregnant women encouraging them to embark on routine iron therapy as prescribed.
Study limitations
The limitations of this study include the fact that only PubMed was used for data extraction. Although PubMed is regarded as one of the most outstanding and globally recognized easily assessable databases for health sciences publications, our inability to search other databases may have resulted in missing additional relevant publications. Another limitation of this study has to do with the scope of the reviewed publications. Every study reviewed was conducted only in a section of Nigeria. Consequently, it may be inappropriate to generalize the findings because of the diverse socioeconomic and cultural settings of Nigeria. There may be a need to repeat some of the studies in other parts of the country to see if there will be similar or contrary outcomes. Some risk factors for an iron deficiency which are common in developing countries, for example, parasitic infestations and chronic diseases were not assessed for. Furthermore, upset gastro intestine which is common during pregnancy and may have contributed to poor compliance to routine iron therapy was not assessed.
Conclusion
The prevalence of iron deficiency anemia in pregnancy is still high in Nigeria. Risk factors associated with iron deficiency anemia include multiparity, third trimester of pregnancy, and poor socioeconomic status (low educational attainment, poor economic status, occupation, poor living condition). Factors associated with poor compliance to routine iron therapy include non-utilization of antenatal care services, low educational attainment, distance to a health facility, single and teenage mother, increasing age, and living in the rural area. There should be continuous awareness creation and health education on the importance of utilization of antenatal care services as well as family planning services, provision of health facilities to areas where they are not available to encourage early booking and utilization of antenatal care services, education, and economic empowerment of women.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, et al. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995–2011: A systematic analysis of population-representative data. Lancet Glob Health2013;1:E16-25.
2. Beutler E, Waalen J. The definition of anaemia: What is the lower limit of normal of the blood hemoglobin concentration? Blood 2006;107: 1747- 50.
3. Khaskheli M, Baloch S, Sheeba A, Baloch S, Khaskheli F. Iron deficiency anaemia is still a major killer of pregnant women. Pak J Med Sci 2016;32:630-4. Back to cited text no. 3
4. Steer PJ. Maternal hemoglobin concentration and birth weight. Am J Clin Nutr 2000;71 (5 Suppl):1285S-7S.
5. UNICEF and Micronutrient Initiative. Vitamin and mineral deficiency: A global progress report. 2004.
6. World Health Organisation. Iron deficiency anaemia: Assessment, prevention and control. WHO/ NHD/ 01.3, Geneva, 2001.
7. Lawson JB. Anaemia in pregnancy. In: Lawson JB, Stewart DB, editors. Obstetrics and Gynaecology in the Tropics. London: Edwards Arnold; 1967.
8. Centers for Disease Control. Criteria for anaemia in children and childbearing aged women. Morb Mortal Wkly Rep 1989;38:400-17.
9. Balarajan Y, Ramakrishnan U, Ozaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet 2011; 378:2123-35.
10. Stoltzfus RJ, Mullany L, Black, RE. Iron deficiency anaemia. In: M Ezzati, Lopez AD, Rodgers A, Murray CJL, editors. Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Major Risk Factors. Geneva: World Health Organization; 2004. p. 163-210. Available from: http://www. who.int/publications/cra/chapters/volume1/0163-0210.pdf?ua=1. [Last accessed on 2018 Jul 20].
11. World Health Organization. The Prevalence of Anaemia in Women: A Tabulation of Available Information. 2nd ed. Geneva: WHO; 1992 (WHO /MCH/MSM/ 92.2).
12. Obasi IO, Nwachukwu N. Comparative iron related anaemia at pregnancy in Ebonyi State, South-east Nigeria. J Med Sci 2013;13:425-31.
13. Daru J, Zamora J, Fernandez-Felix BM, Vogel J, Oladapo OT. Risk of matrenal mortality in women with severe anaemia during pregnancy and post-partum: A multilevel analysis. Lancet 2018;6:E548-54.
14. Goonewardene M, Shehata M, Hamad A. Anaemia in pregnancy. BestPract Res Clin Obstet Gynaecol 2012;26:3-24.
15. Chandra S, Tripathi AK, Mishra S, Amzarul M, Vaish AK. Physiological changes in hematological parameters during pregnancy. Indian JHematol Blood Transfus 2012;28:144-6.
16. Milman N. Oral iron prophylaxis in pregnancy: Not too little and not too much! J Pregnancy 2012;5:43-5.
17. Abbaspour N, Hurrell R, Kelishadi R. Review on iron and its importance for human health. J Res Med Sci 2014;19:164-74.
18. UNFPA. Sub-Saharan Africa’s maternal death rate down 41 per cent. 2010. Available from: http://africa. unfpa.org/public/cache/offonce/news/pid/10767. [Last accessed on 2017 Aug 15].
19. Brabin BJ, Hakimi M, Pelletier D. An analysis of anaemia and pregnancy related maternal mortality. J Nutr 2001;131:604S-15S.
20. Dim CC, Onah HE. The prevalence of anaemia among pregnant women at booking in Enugu, South Eastern Nigeria. Med Gen Med 2007;9:11.
21. Esike CO, Anozie OB, Onoh RC, Sunday UC, Nwokpor OS, Umeora OU. The prevalence of anaemia in pregnancy at booking in Abakaliki, Nigeria. Trop J Obstet Gynaecol 2016;33:332-6.
22. Mekonnen FA, Ambaw YA, Neri GT. Socio-economic determinants of anaemia in pregnancy in North Shoa Zone, Ethiopia. PLoS One 2018;13 :e0202734.
23. Hassan AA, Mamman AI, Adaji S, Musa B, Kene S. Anaemia and iron deficiency in pregnant women in Zaria, Nigeria. Sub-Saharan Afr J Med 2014;1:36-9.
24. Okafor LA, Dieiomaoh FM, Oronsaye AU. Bone marrow status of anaemic pregnant women on supplemental iron and folic acid in a Nigerian community. Angiology 1985;36:500-3.
25. Oluboyede OA, Topley E, Ogunbode O. iron deficiency in pregnant women in Ibarapa District of Western Nigeria. Br J Haematol 1977;36: 527-31.
26. Okafor IM, Okpokam DC, Antai, AB, Usanga EA. Iron status of pregnant women in rural and urban communities of Cross River State, South Nigeria. Niger J Physiol Sci 2017;31:121-5.
27. Isah HS, Fleming AF, Ujah IA, Ekwempu CC. Anaemia and iron status of pregnant and non-pregnant women in the guinea savanna of Nigeria. Ann Trop Med Parasitol 1985;79: 485-93.
28. Al-Farsi YM, Brooks DR, Werler MM, Cabral HJ, Al-Shafei MA, Wallenburg HC. Effect of high parity on occurrence of anaemia in pregnancy: A cohort study. BMC Pregnancy Childbirth 2011;11:7.
29. Zavaleta N, Caulfield LE, Garcia T. Changes in iron status during pregnancy in Peruvian women receiving prenatal iron and folic acid supplements with or without zinc. Am J Clin Nutr 2000;71:956-61.
30. Ofojekwu MN, Nnanna OU, Okolie CE, Odewumi LA, Isiguzoro IO, Lugos MD. Hemoglobin and serum iron concentration in menstruating nulliparous women in Jos, Nigeria. Lab Med 2013;44:121-4.
31. Ribot B, Aranda N, Viteri F, Hernandez-Martinez C, Canals J, Arija V. Depleted iron stores without anaemia early in pregnancy carries increased risk of lower birth weight even when supplemented daily with moderate iron. Hum Reprod 2012;27:1260-6.
32. Percy L, Mansour D. Iron deficiency and iron deficiency anaemia in women’s health. Obstet Gynaecol 2017;19:155-61.
33. Amah-Tariah FS, Ojeka SO, Dapper DV. Haematological values in pregnant women in Port Harcourt, Nigeria II: Serum iron and transferring, total and unsaturated iron binding capacity and some red cell and platelet indices. Niger J Physiol Sci 2011;26:173-8.
34. Zondervan HA, Oosting J, Hardeman MR, Smorenberg-Schoorl ME, Treffers PE. The influence of maternal whole blood viscosity on fetal growth. Eur J Obstet Gynecol Reprod Biol 1987;25:187-94.
35. Soma-Pillay P, Nelson-Piercy C, Tolppanen H, Mebazaa A. Physiological changes in pregnancy. Cardiovasc J Afr 2016;27:89-94.
36. Fisher AL, Nemeth E. Iron homeostasis during pregnancy. Am J Clin Nutr 2017;106(Suppl):1567S-74S.
37. Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutri 2000;72 (Suppl):257S-64S.
38. Gautam CS, Saha L, Sekhri K, Saha PK. Iron deficiency in pregnancy and the rationality of iron supplements prescribed during pregnancy. Medscape J Med 2008;10:283.
39. Ndukwu GU, Dienye PO. Prevalence and socio-demographic factors associated with anaemia in pregnancy in a primary health centre in Rivers State, Nigeria. Afr J Prim Health Care Fam Med 2012;4:328.
40. Owolabi MO, Owolabi AO, Olaolorun DA. Sociodemographic factors in anaemia in pregnancy in south-western Nigeria. S Afr Fam Pract 2012;54:222-7.
41. Nwonwu EU, Ibekwe PC, Ugwu JI, Obarezi HC, Nwagbara OC. Prevalence of malaria parasitaemia and malaria related anaemia among pregnant women in Abakaliki, South east Nigeria. Niger J Clin Pract 2009;12:182-6.
42. Onyeneho NG, Aronu NI, Chukwu N, Agbawodikeizu UP, Malgorzata CM, Subramanian SV. Factors associated with compliance to recommended micronutrients uptake for prevention of anaemia during pregnancy in urban, peri-urban, and rural communities in Southeast Nigeria. J Health Popul Nutr 2016;35:35.
43. Dairo MD, Lawoyin TO. Demographic factors determining compliance to iron supplementation in pregnancy in Oyo State, Nigeria. Niger J Med 2006;15:241-4.
44. Osungbade K, Oginni S, Olumide A. Content of antenatal care services in secondary health facilities in Nigeria: Implication for quality of maternal health care. Int J Qual Health C 2008;20:346-51.
45. Ali NR, Luby S, Hossein RM. Does use of a government service depend on distance from the health facility? Health Policy Plann 1999;14:191-7.
46. Onasoga OA, Afolayan JA, Oladimeij BD. Factors influencing utilization of antenatal care services among pregnant women in Ife Central LGA, Osun State Nigeria. Adv Appl Sci Res 2012;3:1309-15.
47. Ugwu EO, Olibe AO, Obi SN, Ugwu AO. Determinants of compliance to iron supplementation among pregnant women in Enugu, Southeastern Nigeria. Niger J Clin Pract 2014;17:608-12.
48. Hambali IU, Kodomi QG, Nelson L, Martins SD, Hambali MU, Kodomi YG, et al. Factors contributing to non-compliance to routine ante-natal haematinics among pregnant women attending ante-natal clinic in University of Maiduguri Teaching Hospital, Borno, Nigeria. Int J Reprod Contracept Obstet Gynecol 2016;5:3824-31.
49. Selvaraj K, Arumugasamy P, Sarkar S. Compliance and patterns of iron-folic acid intake among adolescent girls and antenatal women in rural Tamil Nadu. Chrismed J Health Res 2017;4:87-93.
50. Kamau MW, Mirie W, Kimani S. Compliance with Iron and folic acid supplementation (IFAS) and associated factors among pregnant women: Results from a cross-sectional study in Kiambu County, Kenya. BMC Public Health 2018;18:580.
51. Nisar YB, Alam A, Aurangzeb B, Dibley MJ. Perceptions of antenatal iron-folic acid supplements in urban and rural Pakistan: A qualitative study. BMC Pregnancy Childbirth 2014;14:344.
52. Lutsey PL, Dawe D, Vilate E, Valencia S, Lopez O. Iron supplementation compliance among pregnant women in Bicol, Philippines. Public Health Nutr 2007;11:76-82.
53. Adanikin AI, Awoleke JO, Olofinbiyi BA, Adanikin PO, Ogundare OR. Routine iron supplementation and anaemia by third trimester in a Nigerian Hospital. Ethiop J Health Sci 2015;25:305-11.