Oseni, TIA; Emonriken, A1; Ahmed, SD1; Dic-Ijiewere, M1
Department of Family Medicine, Ambrose Alli University, Ekpoma, Edo State, Nigeria
1Department of Internal Medicine, Irrua Specialist Teaching Hospital, Irrua, Edo State, Nigeria
Address for correspondence: Dr. TIA Oseni, Department of Family Medicine, Ambrose Alli University, Ekpoma, Edo State, Nigeria. E-mail: tijanioseni@yahoo.com
Abstract
Background:
Hypertension (HTN) is the commonest cardiovascular risk factor in sub-Saharan Africa. It is a global public health threat, often associated with significant morbidities and mortality with rising prevalence both in rural and semi-urban areas of economically disadvantaged countries.
Aim:
This study aimed to assess the determinants of blood pressure control among patients with hypertension receiving care at the Irrua Specialist Teaching Hospital in Southern Nigeria.
Patients and Methods:
A cross-sectional study of 502 consenting hypertensive adults receiving care at the Irrua Specialist Teaching Hospital, Irrua in Edo State, South-south Nigeria. A pre-tested semi-structured interviewer-administered questionnaire was used to collect data which was analyzed using SPSS version 21 and the level of significance was set at P < 0.05.
Results:
Five hundred and two participants (226 males, 276 females) completed the study with a mean age of 52.98 ± 12.82 years. Optimal blood pressure control was found in 15.5% of the study participants. Blood pressure control was significantly associated with being married (OR 1.549, CI: 1.040-2.309), having a monthly household income of over N50,000 (OR 1.691, CI: 0.999-2.863), engaging in physical activity (OR = 1.537, CI: 0.989-2.388), and not being obese evidenced by a normal Waist Hip Ratio (OR = 2.276, CI: 1.555-3.332).
Conclusion:
Blood pressure control to target goal was low in the study population and achieved only in less than one-fifth of respondents on antihypertensive therapy. Numerous socio-demographic and lifestyle variables were shown to be associated with blood pressure control. Physicians should emphasize medication adherence and lifestyle modification approaches in hypertensive adults.
Keywords:
Blood pressure; control; determinants; hypertension; rural
INTRODUCTION
Hypertension is a health condition of global concern.1 It is the most common cardiovascular risk factor in sub-Saharan Africa.2 It is a major risk factor for heart failure, stroke, and kidney failure.3 The prevalence of hypertension in Nigeria from the meta-analysis of studies between 1980 and 2013 is put at 28.9% with a projected prevalence rate of 30.8% by the year 2030.4 Lifestyle factors like obesity, physical inactivity, a diet high in salt and unsaturated fats, and social habits like alcohol consumption and cigarette smoking contribute to the rising prevalence of hypertension globally.1,4,5
Modification of dietary habits and physical activity is of utmost importance in the non-pharmacological management of hypertension. They are also beneficial in controlling and preventing other comorbidities that increase cardiovascular risk. Significant reductions in systolic blood pressure (SBP) and diastolic blood pressure (DBP) which can be sustained up to 24 hours after exercise have been observed in individuals who partake in exercise.6–9
Uncontrolled hypertension leads to severe cardiovascular diseases, renal failure, and mortality.10 Blood pressure (BP) levels have been proven to be directly associated with the risk of coronary heart disease and stroke recurrence.11 Furthermore, the link between blood pressure and the risk of cardiovascular disease events is independent of other risk factors, implying that the higher the blood pressure, the higher the risk of heart failure, and end-stage renal disease.11 High blood pressure is associated with at least 7.6 million deaths per year worldwide (13.5% of all deaths), making it the leading risk factor for cardiovascular diseases.12 Despite the availability of multiple effective antihypertensive medications with proven benefits in reducing cardiovascular morbidity and mortality, control of hypertension remains poor.10,12 In both high and low-income countries, less than 27% and 10%, respectively, of hypertensive patients have achieved their target blood pressure.13,14
The aim of this study was to assess the determinants of blood pressure control among hypertensives receiving treatment in our facility. This will guide patients’ education on the appropriate measures that will help them achieve better blood pressure control and reduce morbidities associated with poor control.
METHODOLOGY
This was a descriptive cross-sectional study conducted in the general and medical outpatient clinics of Irrua Specialist Teaching Hospital, Irrua, a rural community in Edo State, Southern Nigeria. Systematic sampling was used to recruit 502 consenting adults who were diagnosed with hypertension for at least one year. The study was conducted over a three-month period (January to March 2021).
A semi-structured interviewer-administered pre-tested questionnaire was used to collect data from respondents. Blood pressure was measured with an Omron digital sphygmomanometer (OMRON M2 Classic Intellisense) and the mean of three readings 10 minutes apart was recorded. Blood pressure less than 140/90 mmHg was classified as controlled while those greater than 140/90 mmHg were classified as uncontrolled. Waist circumference was determined using a non-stretchable tape placed midway between the coastal margin and the iliac crest. Hip circumference was determined using the same tape at the level of the greater trochanter. Waist Hip Ratio (WHR) was determined by dividing the waist circumference by the hip circumference and WHR <1.0 for men and <0.9 for women were classified as normal while those with a Waist Hip Ratio of >1.0 for men and >0.9 for women were classified as obese.
The data were analyzed using the Statistical Package for Social Sciences (SPSS) version 21 and the level of significance was set at P < 0.05. Ethical approval was obtained from the ethics department of Irrua Specialist Teaching Hospital and written informed consent was obtained from respondents after a detailed explanation of the study and procedures to them.
Operational definitions
In line with the World Health Organization and the Joint National Committee on Prevention, Detection Evaluation, and Treatment of high blood pressure,10,15 Hypertension was defined as SBP greater than or equal to 140 mmHg and/or DBP greater than or equal to 90 mmHg or being on drug therapy for hypertension.
Participants whose BP was less than 140/90 mmHg were classified as controlled (Optimal control for BP ≤120/80 mmHg and fair control for BP between 120/80 and <140/90 mmHG) while those with BP greater than 140/90 mmHg were classified as uncontrolled.
Waist Hip Ratio (WHR) of <1.0 for men and <0.9 for women were classified as normal while those with Waist Hip Ratio of >1.0 for men and >0.9 for women were classified as obese.
Consumption of 5 or more servings of fruits and vegetables was considered adequate; a serving of fruit being one medium size of any fruit and a serving of vegetable being a half cup of cooked or raw vegetable. Excessive salt was defined as intake of greater than 5 g per day according to WHO and this was assessed by asking respondents whether they added extra salt to food or used much salt in cooking. Fatty meat consumption was defined as the consumption of beef and red meat.
RESULTS
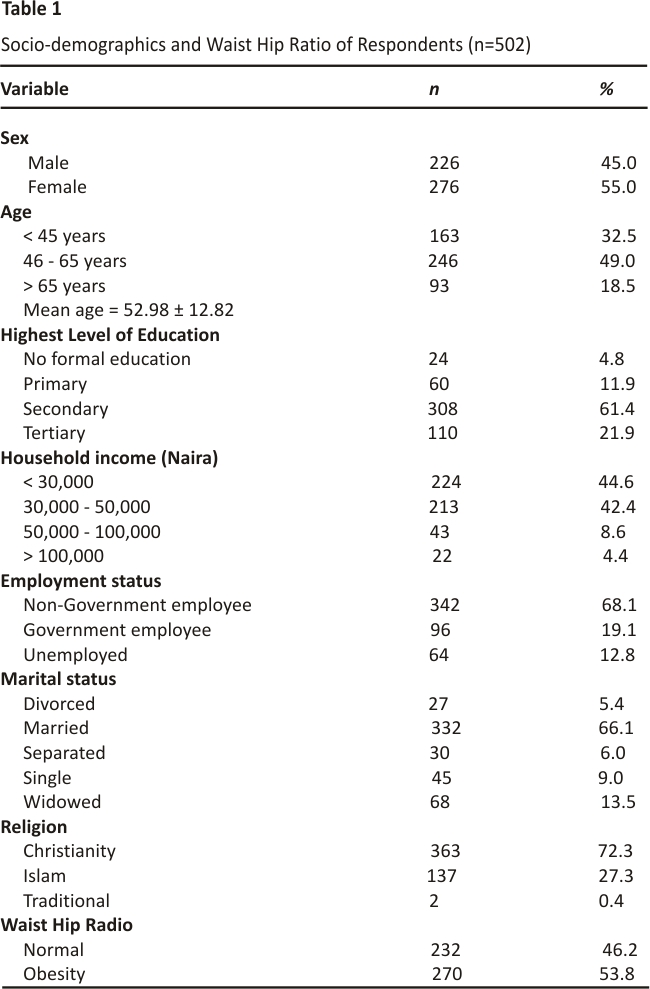
Of the 502 respondents, 55.0% were females, 32.5% were less than 45 years, 49.0% were aged 46-65% and the rest (18.5%) were older than 65 years, while the mean age was 52.98 ± 12.82 years. More than half (61.4%) of respondents had secondary education, 21.9% had tertiary education, 11.9% had primary education while few (4.8%) had no formal education. Quite a number (44.6%) of respondents earned below the national minimum wage of N30,000 per month while few (4.4%) earned above N100,000, and more than half (58.2%) of respondents were Non-Government employees. Most (66.1%) of the respondents were married, 13.5% were widowed, 5.4% were divorced, 72.3% were Christians and 27.3% practiced Islam [Table 1].
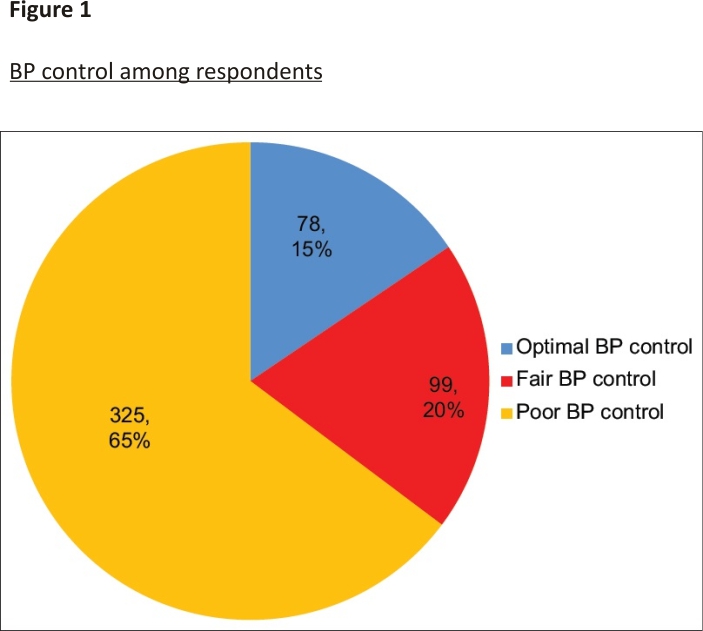
The majority 325 (64.8%) of respondents had poor BP control, while others had fair 99 (19.7%) and optimal 78 (15.5%) BP control, respectively [Figure 1].
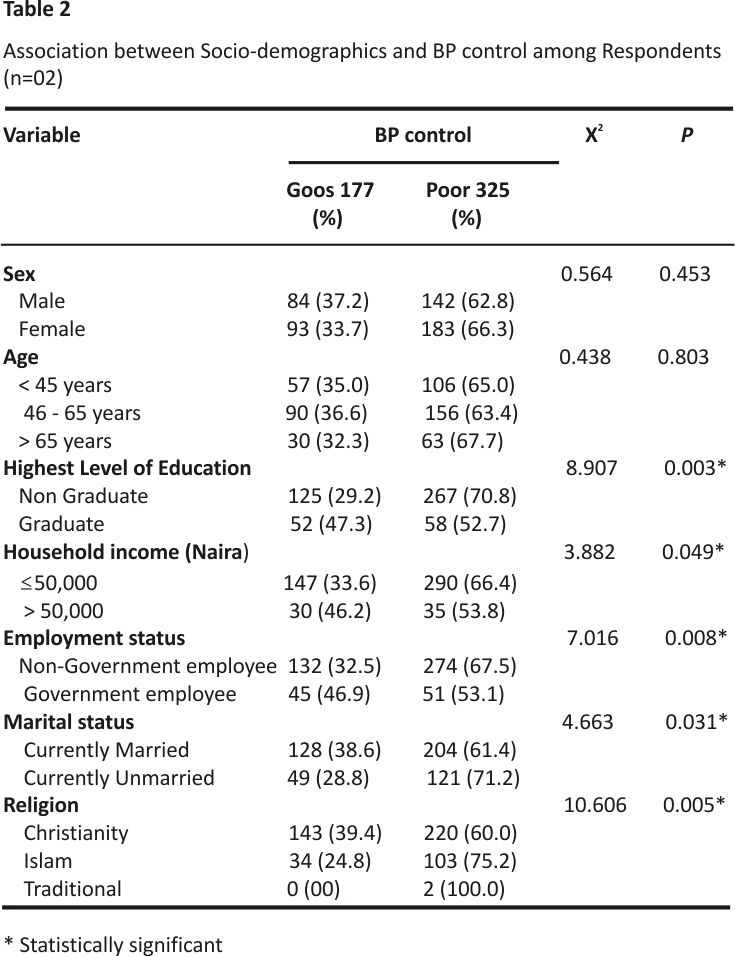
This study found that the highest level of education (p = 0.004), monthly household income (p = 0.028), employment status (p = 0.034), marital status (p = 0.031), and religion (p = 0.005) were significantly associated with BP control [Table 2].
Also, there was a significant association between BP control and level of physical activity (p = 0.039), smoking (p = 0.049), salt consumption (p = 0.015), duration of hypertension (p = 0.004), and Waist Hip Ratio (p < 0.001) [Table 3].
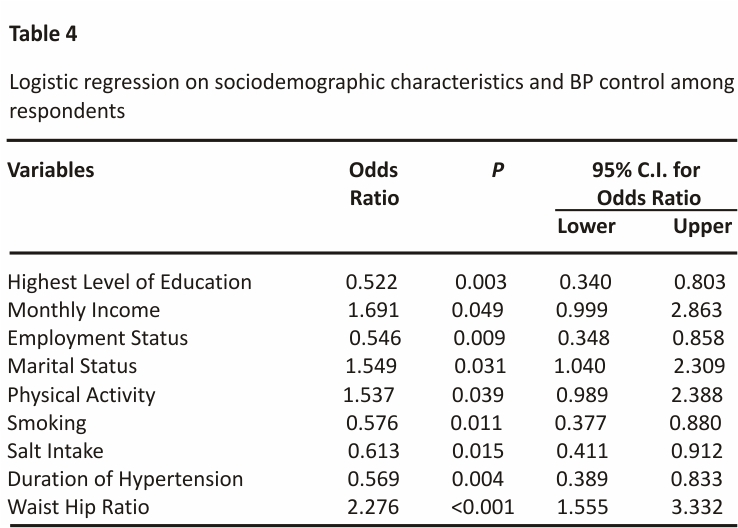
Multiple Logistic Regression was done to determine risk factors for poor BP control while adjusting for associated socio-demographics (education level, household income, employment status, marital status, level of activity, smoking, salt intake, duration of hypertension, and Waist Hip Ratio). Blood pressure was more likely to be controlled in respondents who had a household monthly income of over N 50,000 (OR 1.691, CI: 0.999-2.863), were currently married (OR 1.549, CI: 1.040-2.309), more active physically (OR = 1.537, CI: 0.989-2.388) and had a normal Waist Hip Ratio (OR = 2.276, CI: 1.555-3.332). [Table 4].
DISCUSSION
Blood pressure control to target goal was low in the study population and achieved only in less than one-fifth of respondents on blood pressure lowering medications. This compares to 12.4% and 17.2% in studies conducted in Zaria and Enugu, respectively, at similar tertiary teaching hospital settings.16,17 However, this figure is lower than the results of surveys conducted in tertiary institutions in Port Harcourt (36.69%), Kano (34.5%), Abeokuta (46.4%), and Ilorin (53.3%).18–21 It was also lower than values in some African countries,22–24 Saudi Arabia,25, and Korea.26 The relatively higher percentage of blood pressure control in these studies may be linked to easy access to medications and medical facilities. Overall, the majority (64.8%) of respondents had poor BP control. Although optimum blood pressure control to less than 140/90 mmHg is a primary strategy for reducing death and disability due to cardiovascular disease, it has remained a global challenge. Several studies have also demonstrated the importance of effective blood pressure control. 18,22,27
The patient’s average age was 52.98 years, which was similar to that reported in other research.19,20,28,29 The gender distribution revealed a 55.0 percent female predominance, which is consistent with the findings of earlier studies.20,29–31 This may be due to the superior health-seeking behavior of the female population. In this study, socio-demographic characteristics such as age and gender had no significant correlation with blood pressure regulation. Similarly, age was not associated with blood pressure control in a study conducted in Port Harcourt by Douglas et al.19 Yet in another study, Asgedom et al.,27 in Southwest Ethiopia, discovered that individuals aged 65 years and higher had considerably poorer blood pressure control. In a study conducted in southwestern Nigeria by Ibrahim et al.,32 advanced age and diabetes were significant contributors to poor blood pressure control. In a number of studies, old age has been recognized as a significant risk factor for poor BP control.20,22,27 This could be because the elderly are more prone to having many co-morbidities, which can have a major impact on blood pressure control. Previous research has connected old age to a loss of systemic arterial elasticity, which leads to a rise in systolic blood pressure.20,27 As a result, clinicians caring for elderly hypertensives should look for and manage any concomitant comorbidities.
This study found an association between monthly household income and blood pressure regulation. A lot of our patients were paid less than the federal minimum wage, which may have hampered their capacity to procure medications and follow treatment plans, resulting in poor blood pressure control. In addition, Nigeria’s national health insurance scheme has a low coverage rate.33 Earlier studies showed that patients with hypertension who have health insurance have been demonstrated to have improved drug adherence and blood pressure control.33 This study also found a significant difference in blood pressure control among respondents who were married compared to those who were not married. This could be due to emotional stability associated with marriage as well as spousal support which married couples enjoy.
Respondents who are better educated are more likely to comprehend their ailment and likely resultant complications and stick to their treatment plan. Cheong et al.34 observed that patients with less than a secondary education were more likely to have poor BP management, similar to our findings. In Ido-Ekiti, Ibrahim et al.32 found that working as a government employee provides a source of income for hypertensive patients, allowing them to conduct effective health education and adherence screening as a strategy for lowering cardiovascular risks associated with uncontrolled hypertension. Furthermore, the majority are more likely to be aware of the importance of appropriate healthcare.
The level of physical activity was an important determinant of BP control in this study. In Southwest Ethiopia, Asgedom et al.27 had similar findings. Despite the significant association between physical activity and BP control in our study, it is crucial to note that only a small percentage of participants engaged in any form of physical exercise, which is consistent with earlier results 18,35 In Nigeria35,36 and other parts of the world,37 the practice of regular exercise is suboptimal among hypertensives. Although moderate-intensity exercise has been shown to improve blood pressure control, there are rising concerns about adherence.35–37
Excessive salt intake, tobacco use, and duration of hypertension were all associated with poor blood pressure control in our study. Patients with a greater than 5-year history of hypertension were more likely to have poor blood pressure control. While Asgedom et al.27 found that adding salt to meals was related to uncontrolled blood pressure, however, found no relationship between blood pressure control and duration of hypertension. This, however, contradicts a report in Port Harcourt by Douglas et al.,19 who found no correlation between salt intake and blood pressure control.
In the Port Harcourt study by Douglas et al.,19 alcohol consumption was significantly linked to blood pressure regulation, which contradicts our findings. They discovered that persons who currently consume alcohol are twice more likely to have uncontrolled blood pressure than those who do not.19 This difference in finding may be due to the fact that our study participants were mostly women, and men in our society consume more alcohol. This is crucial because alcohol consumption is a known risk factor for cardiovascular diseases.
Obesity was observed to be associated with blood pressure management in more than half of our respondents. Obesity is a well-known risk for hypertension and this could have a role in the study’s poor blood pressure regulation. Physicians’ lack of emphasis on lifestyle change and non-drug methods may be responsible for the low control rate. As a result, lifestyle modification and non-drug treatment strategies such as education, weight loss, salt restriction, and regular exercise should be emphasized and intensified in the care of our patients.
Limitations
The study was limited by the fact that it was hospital-based and cross-sectional in nature. A sizeable proportion of patients with hypertension in Nigeria patronize patent medicine stores and self-medicate. The response from this study was based on self-report; hence, there may be a recall bias. Also, the study did not evaluate the drug regimen of our respondents to adequately determine the role of medication adherence in blood pressure regulation in this population. The respondent’s comorbidities such as diabetes mellitus and dyslipidemia were also not evaluated. These have been found by several studies to be negative determinants of blood pressure control. 20,21,38
CONCLUSION
Our study established that respondents had a low and unsatisfactory level of BP control. This finding in a tertiary setting may imply that lower levels of healthcare may have lower control rates in this region. Numerous socio-demographic and lifestyle variables were shown to be associated with blood pressure regulation. In patients with hypertension, lifestyle adjustment of risk factors like obesity, as well as non-drug therapy approaches should, necessarily, therefore be emphasized and intensified in addition to adherence to drug treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
1. World Health Organization. A Global Brief on Hypertension: World Health Day Geneva, Switzerland WHO 2013
2. Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: A systematic analysis. PLoS One 2014;9:e104300
3. Ogah OS. Blood pressure, the prevalence of hypertension and hypertension related complications in Nigerian Africans: A review. World J Cardiol 2012;4:327–40
4. Olawuyi AT, Adeoye IA. The prevalence and associated factors of non-communicable disease risk factors among civil servants in Ibadan, Nigeria. PLoS One 2018;13:e 0203587
5. World Health Organization. WHO guidelines on physical activity and sedentary behavior. World Health Organization 2020
6. Nicoll R, Henein MY. Hypertension and lifestyle modification: How useful are the guidelines? Br J Gen Pract 2010;60:879–80
7. Pescatello LS, MacDonald HV, Lamberti L, Johnson BT. Exercise for hypertension: A prescription update integrating existing recommendations with emerging research. Curr Hypertens Rep 2015; 17:87
8. Odunaiya NA, Louw QA, Grimmer KA. Are lifestyle cardiovascular disease risk factors associated with pre-hypertension in 15-18 years rural Nigerian youth? A cross-sectional study. BMC Cardiovasc Disord 2015;15:144
9. Appel LJ. ASH position paper: Dietary approaches to lower blood pressure. J Clin Hypertens 2009;11:358–68
10. Sinnott SJ, Smeeth L, Williamson E, Douglas IJ. Trends for prevalence and incidence of resistant hypertension: Population-based cohort study in the UK 1995– 2015. BMJ 2017;358:j3984 doi:10.1136 /bmj.j3984
11. Anderson KM, Wilson PWF, Odell PM, Kannel WB. An updated coronary risk profile. Circulation 1991;83:356–62
12. Chow CK, Teo KK, Rangarajan S, Islam S, Gupta R, Avezum A, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959– 68
13. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, detection, evaluation, and Treatment of high blood pressure. Hypertension 2003;42: 1206–52
14. Pereira M, Lunet N, Azevedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens 2009;27: 963–75
15. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. The seventh report of the Joint National Committee on Prevention, detection, evaluation, and Treatment of high blood pressure: The JNC 7 Report. JAMA 2003;289:2560–72
16. Oyati A, Orogade A, Danbauchi S, Azuh P. Awareness, treatment and control of hypertension among hypertensives in Zaria. J Med Trop 2011;13:139–44
17. Ezeala-adikaibe B, Mbadiwe N, Okudo G, Nwosu N, Nwobodo N, Onyebueke G, et al. Factors associated with medication adherence among hypertensive patients in a tertiary health center: A cross-sectional study. Arch Community Med Public Health 2017;3:24–31
18. Ojo OS, Malomo SO, Sogunle PT, Ige AM. An appraisal of blood pressure control and its determinants among patients with primary hypertension seen in a primary care setting in Western Nigeria. S Afr Fam Pract 2016;58:192–201
19. Douglas KE, Alabere ID. Blood pressure control and associated factors among hypertensive patients in the University of Port Harcourt teaching hospital in South-South Nigeria. Niger J Med 2018;27:234–44
20. Tamuno I, Babashani M. Blood pressure control amongst hypertensive patients in a tertiary health care facility in Northern Nigeria. Res J Med Sci 2012;6:26–32
21. Olanrewaju TO, Aderibigbe A, Chijioke A, Sanya EO, Busari OA, Kolo PI, et al. Descriptive analysis of blood pressure control among treated hypertensive patients in a tertiary hospital in Nigeria. Afr J Med Med Sci 2011;40:207–12
22. Mutua EM, Gitonga MM, Mbuthia B, Muiruri N, Cheptum JJ, Maingi T. Level of blood pressure control among hypertensive patients on follow-up in a Regional Referral Hospital in Central Kenya. Pan Afr Med J 2014;18:278
23. Menanga A, Edie S, Nkoke C, Boombhi J, Musa AJ, Mfeukeu LK, et al. Factors associated with blood pressure control amongst adults with hypertension in Yaounde, Cameroon: A cross-sectional study. Cardiovasc Diagn Ther 2016;6: 439–45
24. Ambaw AD, Alemie GA, Wyohannes SM, Mengesha ZB. Adherence to antihypertensive treatment and associated factors among patients on follow-up at University of Gondar Hospital, Northwest Ethiopia. BMC Public Health 2012;12:282
25. Al Ghobain M, Alhashemi H, Aljama A, Bin Salih S, Assiri Z, Alsomali A, et al. Nonadherence to antihypertensive medications and associated factors in general medicine clinics. Patient Prefer Adherence 2016;10:1415–9
26. Yang MH, Kang SY, Lee JA, Kim YS, Sung EJ, Lee KY, et al. The effect of lifestyle changes on blood pressure control among hypertensive patients. Korean J Fam Med 2017; 38:173–80
27. Asgedom SW, Gudina EK, Desse TA. Assessment of blood pressure control among hypertensive patients in Southwest Ethiopia. PLoS One 2016;11:e0166432
28. Akpa MR, Alasia DD, Emem-Chioma PC. An appraisal of hospital-based blood pressure control in Port Harcourt, Nigeria. Niger Health J 2008;8:27–30
29. Abdu A, Lawrence AB, Shuaibu AT, Sani T. Blood pressure control among hypertensive subjects in Dutse, Northwestern Nigeria. Ann Ib Postgrad Med 2019;17: 59–64
30. Gebrihet TA, Mesgna KH, Gebregiorgis YS, Kahsay AB, Weldehaweria NB, Weldu MG. Awareness, treatment, and control of hypertension are low among adults in Aksum town, northern Ethiopia: A sequential quantitative-qualitative study. PLoS One 2017;12:e0176904
31. Achieng’ L, Joshi MD, Ogola EN, Karari E. Adequacy of blood pressure control and level of adherence with antihypertensive therapy. East Afr Med J 2009; 86:499–506
32. Ibrahim AO, Agbesanwa TA, Shabi OM, Omosanya OE, Ismail WH, Deji-Dada OO. Blood pressure control and its associated factors among hypertensive patients in a federal teaching hospital, ido- ekiti, Southwest Nigeria. Arch Community Med Public Health 2020;6:167–73
33. Hendriks ME, Rosendaal NTA, Wit FWNM, Bolarinwa OA, Kramer B, Brals D, et al. Sustained effect of health insurance and facility quality improvement on blood pressure in adults with hypertension in Nigeria: A population-based study. Int J Cardiol 2016;202: 477–84
34. Cheong AT, Sazlina SG, Tong SF, Azah AS, Salmiah S. Poor blood pressure control and its associated factors among older people with hypertension: A cross-sectional study in six public primary care clinics in Malaysia. Malays Fam Physician 2015;10:19–25
35. Iloh GUP, Ofoedu JN, Njoku PU, Amadi AN, Godswill-Uko EU. Medication adherence and blood pressure control amongst adults with primary hypertension attending a tertiary hospital primary care clinic in Eastern Nigeria. Afr J Prim Health Care Fam Med 2013;5:1–6
36. Katibi IA, Olarinoye JK, Kuranga SA. Knowledge and practice of hypertensive patients as seen in a tertiary hospital in the middle belt of Nigeria. Niger J Clin Pract 2010;13:159–62
37. Alsairafi M, Alshamali K, Al-rashed A. Effect of physical activity on controlling blood pressure among hypertensive patients from Mishref Area of Kuwait. Eur J Gen Med 2010;7:377–84
38. Van Den Berg N, Meinke-Franze C, Fiss T, Baumeister SE, Hoffmann W. Prevalence and determinants of controlled hypertension in a German population cohort. BMC Public Health 2013;13:594
Credits: Oseni, TIA; Emonriken, A1; Ahmed, SD1; Dic-Ijiewere, M1. Determinants of Blood Pressure Control among Hypertensive Patients Attending a Rural Teaching Hospital in Southern Nigeria. Nigerian Journal of Clinical Practice 26(3):p 260-266, March 2023. | DOI: 10.4103/njcp. njcp_ 1678_21